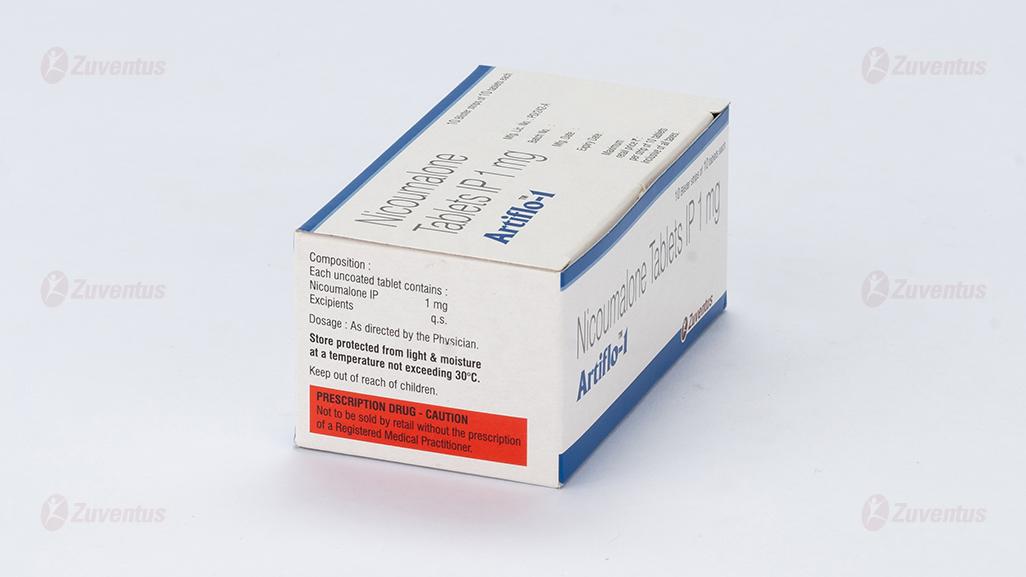
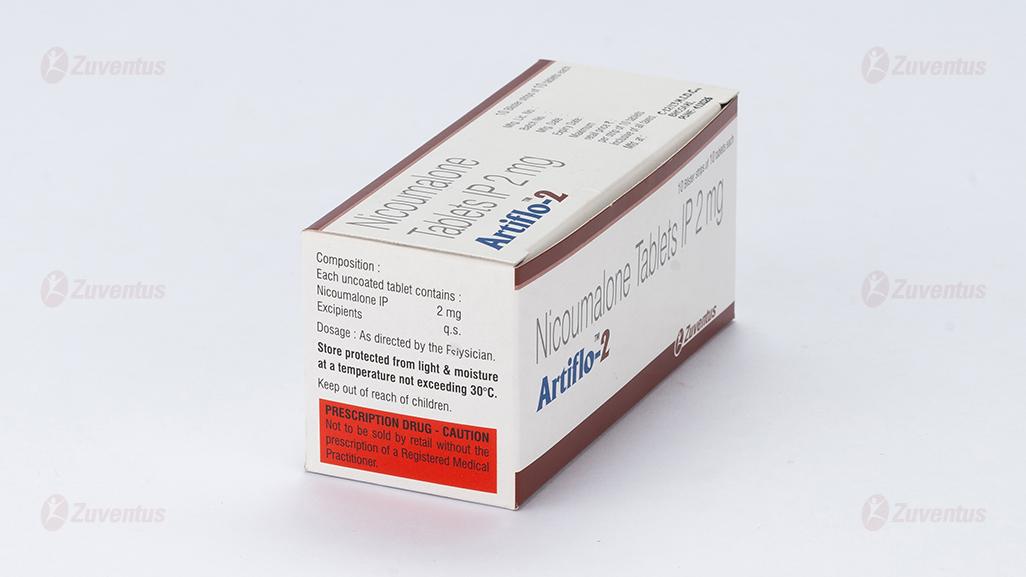
Artiflo
Therapy Area
Cardiology
Generic Name
Nicoumalone Tablets IP 1 mg/2mg/3 mg/4 mg
Qualitative and quantitative composition
Each uncoated tablet contains
Nicoumalone IP 1mg/2 mg/3 mg/4 mg
Excipients q.s
Dosage form and strength
Tablets for oral administration.
1 mg/2 mg/3 mg/4 mg
Clinical particulars
Therapeutic indication
For the prevention and treatment of thromboembolic diseases such as venous thrombosis, atrial fibrillation with embolization, pulmonary embolism and as an adjunct in the treatment of coronary occlusion.
Posology and method of administration
Posology
General target population
Sensitivity to anticoagulants varies from patient to patient and may also fluctuate during the course of treatment. Therefore, it is essential to perform regular testing of prothrombin time (PT)/International Normalised Ratio (INR) and to adjust the patient's dosage accordingly. If this is not possible, Artiflo should not be used. Artiflo should be given in a single oral dose.
Initial dosage:
The dosingof Artiflo must be individualised. If the PT/INR value is within the normal range before starting treatment, the following dosage schedule is recommended:
- The usual starting dose is between 2 mg/day to 4 mg/day without administration of a loading dose.
- Treatment may also be initiated with a loading dose regimen, usually 6 mg on the first day followed by 4 mg on the second day.
If the initial thromboplastin time is abnormal, treatment should be instituted with caution.
Elderly patients (≥65), patients with liver disease or severe heart failure with hepatic congestion or malnourished patients may require lower doses during treatment initiation and maintenance. Measurement of the thromboplastin time should be carried out daily in hospital starting from second or third dose of Artiflo and up to the time when the coagulation status is stabilized within the target range. The interval between tests can later be extended, depending on the stability of PT/INR results. Blood samples for laboratory tests should always be taken at the same time of day.
Maintenance therapy and coagulation tests
The maintenance dose of Artiflo varies from patient to patient and must be checked individually on the basis of PT/INR values. PT/INR should be assessed at regular intervals, i.e. at least once a month. The maintenance dose generally lies between 1 to 8mg daily depending on the individual patient, the underlying disease, clinical indication and desired intensity of anticoagulation.
Depending on the clinical indication, the optimal intensity of anticoagulation or therapeutic range to be aimed at generally lies between INR values of 2.0 and 3.5 (see Table 1). Higher INR values up to 4.5 may be required in individual cases. Table 1 Recommended INR* for Oral Anti-coagulant Therapy
| Indication | Recommended INR |
| Prophylaxis and treatment of venous thromboembolism (including pulmonary embolism) | 2.0 – 3.0 |
| Atrial fibrillation | 2.0 – 3.0 |
| Post-myocardial infarction (with increased risk for thromboembolic complications) | 2.0 – 3.0 |
| Bioprosthetic heart valves | 2.0 – 3.0 |
| Secondary prophylaxis in patients with antiphospholipid syndrome | 2.0 – 3.0 |
| Antiphospholipid syndrome patients with venous thromboembolism on therapeutic vitamin K antagonist | 2.0 – 3.5 |
| Mechanical heart valves | 2.0 – 3.5 |
*The PT, which reflects the reduction of Vitamin K dependent clotting factors VII, X and II, is dependent on the responsiveness of the thrombosplastin used for PT-testing. The responsiveness of the respective local thromboplastin compared to World Health Organisation international reference preparations is reflected by its International Sensitivity Index (ISI). The “International Normalised Ratio” (INR) was introduced for the purpose of standardisation of the PT. The INR is the ratio of the patient's anticoagulated plasma PT to the normal plasma PT using the same thromboplastin in the same test system raised to the power of a value defined by the International Sensitivity Index.
Treatment discontinuation
Generally, after withdrawal of Artiflo, there is usually no danger of reactive hypercoagulability and therefore it is not necessary to give gradually diminishing doses. However, in extremely rare cases, in some high risk patients (e.g. after myocardial infarction), withdrawal should be gradual.
Missed dose
The anticoagulant effect of Artiflo persists beyond 24 hours. If the patient forgets to take the prescribed dose of Artiflo at the scheduled time, the dose should be taken as soon as possible on the same day. The patient should not double the daily dose to make up for a missed dose, but should refer back to his or her doctor.
Conversion from heparin therapy
In clinical situations which require rapid anticoagulation, initial treatment with heparin is preferred since the anticoagulant effect of Artiflo is delayed. Conversion to Artiflo may begin concomitantly with heparin therapy or may be delayed depending on the clinical situation. To ensure continuous anticoagulation, it is advisable to continue to prescribe full dose heparin therapy for at least 4 days after initiation of Artiflo and to continue heparin therapy until the INR has been in the target range on at least two consecutive days. During the transition phase close monitoring of anticoagulation is necessary.
Treatment during dentistry and surgery
Patients on Artiflo, who undergo surgical or invasive procedures require close surveillance of their coagulation status. Under certain conditions, e.g. when the operation site is limited and accessible to permit effective use of local procedures for haemostasis, dental and minor surgical procedures may be performed during continued anticoagulation, without undue risk of haemorrhage. The decision to discontinue Artiflo, even for a short period of time, should carefully consider individual risks and benefits. The introduction of bridging anticoagulant treatment, e.g. with heparin should be based on careful assessment of the expected risks of thromboembolism and bleeding.
Special populations
Renal impairment
Artiflo is contraindicated in patients with severe renal impairment due to an increased risk of haemorrhage. Caution should be exercised in patients with mild to moderate renal impairment.
Hepatic impairment
Artiflo is contraindicated in patients with severe hepatic impairment due to an increased risk of haemorrhage. Caution should be exercised in patients with mild to moderate hepatic impairment.
Paediatric population
Experience with oral anticoagulants including nicoumalone in children remains limited. Caution and more frequent monitoring of PT/INR is recommended.
Elderly
A dose lower than the recommended adult dose may be sufficient in elderly patients. caution and more frequent monitoring of PT/INR is recommended.
Method of administration
The daily dosage should always be taken at the same time of day. The tablet should be swallowed whole with a glass of water.
Contraindications
- Known hypersensitivity to nicoumalone and related coumarin derivatives or to any of the excipients of Artiflo.
- Pregnancy
- Patients unable to co-operate and who are unsupervised (e.g. unsupervised senile patients, alcoholics and patients with psychiatric disorders).
Artiflo is also contraindicated in conditions where the risk of haemorrhage is greater than the possible clinical benefit, e.g.
- Haemorrhagic diathesis or haemorrhagic blood dyscrasias
- Shortly before or after surgical interventionon the central nervous system as well as the eyes and traumatising surgery involving extensive exposure of the tissues
- Peptic ulcers or haemorrhage in the gastro-intestinal tract, urogenital tract or respiratory system; cerebrovascular haemorrhages; acute pericarditis; pericardial effusion; infective endocarditis
- Severe hypertension (due to occult risks)
- Severe hepatic impairment
- Severe renal impairment
- Increased fibrinolytic activity as encountered after operations on the lung, prostate or uterus etc.
Special warnings and precautions for use
Hepatic impairment
Caution should be exercised in patients with mild to moderate hepatic impairment since the synthesis of blood coagulation factors may be impaired or there may be an underlying platelet dysfunction.
Renal impairment
Due to the possibility of accumulation of metabolites in impaired renal function, caution should be exercised in patients with mild to moderate renal impairment.
Heart failure
In severe heart failure, a very cautious dosage schedule must be adopted, since hepatic congestion may reduce the activation of gamma-carboxylation of coagulation factors. However, with reversal of the hepatic congestion, it may be necessary to raise the dosage.
Haematological
Caution should be exercised in patients with known or suspected (e.g. abnormal bleeding after injury) protein C or protein S deficiency.
Calciphylaxis
Calciphylaxis is a rare syndrome of vascular calcification with cutaneous necrosis, associated with high mortality. The condition is mainly observed in patients with end-stage renal disease on dialysis or in patients with known risk factors such as protein C or S deficiency, hyperphosphataemia, hypercalcaemia or hypoalbuminaemia. Rare cases of calciphylaxis have been reported in patients taking vitamin K antagonists including Artiflo also in the absence of renal disease. In case calciphylaxis is diagnosed, appropriate treatment should be started and consideration should be given to stopping treatment with Artiflo.
Hemorrhage
Artiflo can cause major (including hemorrhagic and hypovolemic shock) or fatal bleeding. Risk factors for bleeding include high intensity of anticoagulation (INR >4.0), age ≥ 65, history of highly variable INRs, history of gastrointestinal bleeding, hypertension, cerebrovascular disease, serious heart disease, anemia, malignancy, trauma, renal insufficiency, concomitant drugs, Regular monitoring of INR should be performed on all treated patients. Those at high risk of bleeding may benefit from more frequent INR monitoring, careful dose adjustment to desired INR, and a shorter duration of therapy.
Special populations
In paediatric and elderly patients (≥65 years), caution and more frequent monitoring of PT/INR is recommended (Posology and method of administration and Pharmacokinetic properties).
Miscellaneous
Strict medical supervision should be given in cases where the disease or condition may reduce the protein binding of Artiflo (e.g. thyrotoxicosis, tumours, renal disease, infections and inflammation). Disorders affecting gastro-intestinal absorption may alter the anticoagulant activity of Artiflo. During treatment with anticoagulants, intramuscular injections may cause haematomas and should be avoided. Subcutaneous and intravenous injections may be given without such complications. Meticulous care should be taken where it is necessary to shorten the PT/INR (thromboplastin time) for diagnostic or therapeutic procedures (e.g. angiography, lumbar puncture, minor surgery, tooth extractions etc.). Patients with rare hereditary problems of galactose intolerance, the Lapp lactase deficiency or glucose-galactose malabsorbtion should not take this medicine.
Interaction with other medicinal products and other forms of interaction
There are many possible interactions between coumarins and other drugs; those of clinical relevance are given below. Many of these are isolated reports only or have been reported with warfarin rather than nicoumalone; for completeness, all have been included. The mechanisms of these interactions include disturbances of absorption, inhibition or induction of the metabolising enzyme system (mainly CYP2C9), and reduced availability of vitamin K1, necessary for gamma-carboxylation of prothrombin–complex factors. It is important to note that some drugs may interact by more than one mechanism. Every form of therapy may involve the risk of an interaction, although not all will be significant. Thus, careful surveillance is important and frequent coagulation tests (e.g. twice weekly) should be carried out when initially prescribing any drug in combination with Artiflo, or when withdrawing a concomitantly administered drug. Interactions resulting in concomitant use not being recommended The following drugs potentiate the anticoagulant activity of nicoumalone and/or alter haemostasis and thereby increase the risk of haemorrhage: Drugs altering haemostasis may potentiate the anticoagulant activity of Artiflo and thereby increase the risk of haemorrhage. Consequently, Artiflo should not be prescribed with such drugs, which include:
- heparin (including LMWH) (except in situations which require rapid anticoagulations); • antibiotics (e.g. clindamycin);
- platelet-aggregation inhibitors (e.g. dipyridamole, clopidogrel), salicyclic acid and its derivatives, (e.g. acetylsalicylic acid, para-aminosalicylic acid, diflunisal);
- clopidogrel, ticlopidine, phenylbutazone or other pyrazolone derivatives (e.g. sulfinpyrazone), and other non-steroidal anti-inflammatory drugs (NSAIDs) including COX-2 inhibitors (e.g. celecoxib), high dose IV methylprednisolone. Increased INR has been reported in patients taking glucosamine and oral vitamin K antagonists. Patients treated with oral vitamin K antagonists should therefore be closely monitored at the time of initiation or termination of glucosamine therapy. The risk of gastrointestinal haemorrhage is increased if Artiflo is prescribed in combination with these substances. In the case of unavoidable concurrent use, coagulation tests should be performed more frequently.
Interactions to be considered
The anticoagulant effect may be potentiated by concomitant administration of the following drugs:
- allopurinol;
- anabolic steroids;
- androgens;
- anti-arrhythmic agents (e.g. amiodarone, quinidine);
- antibiotics:
- broad spectrum antibiotics (e.g. amoxicillin, co-amoxiclav) macrolides (e.g. erythromycin, clarithromycin);
- cephalosporins second and third generation;
- metronidazole;
- quinolones (e.g. ciprofloxacin, norfloxacin, ofloxacin);
- tetracyclines;
- neomycin;
- chloramphenicol.
- imidazole derivatives, including topical administration (e.g. econazole, fluconazole, ketoconazole, miconazole);
- sulfonamides (including co-trimoxazole);
- fibrates (e.g. clofibric acid), its derivatives and structural analogues (e.g. fenofibrate, gemfibrozil);
- disulfiram;
- etacrynic acid;
- glucagon;
- oral antidiabetics (e.g. glibenclamide);
- sulphonylureas (such as tolbutamide and chlorpropamide);
- H2 antagonists (e.g. cimetidine);
- paracetamol;
- thyroid hormones (including dextrothyroxine);
- sulfinpyrazone;
- statins (e.g. atorvastatin, fluvastatin, simvastatin);
- selective serotonin re-uptake inhibitors (e.g. citalopram,fluoxetine, sertraline,paroxetine);
- tamoxifen;
- 5-fluorouracil and analogues;
- tramadol;
- proton pump inhibitors (e.g. omeprazole);
- plasminogen activators (e.g. urokinase; streptokinase and alteplase);
- thrombin inhibitors (e.g. argatroben);
- prokinetic agents (e.g. cisapride);
- antacids (e.g. magnesium hydroxide);
- viloxazine.
- Inhibitors of CYP2C9 may potentiate the anticoagulant effect of nicoumalone. The anticoagulant effect may be diminished by concomitant administration of the following drugs:
- aminoglutethimide;
- antineoplastic drugs (e.g. azathioprine, 6-mercaptopurine);
- barbiturates (e.g. Phenobarbital);
- carbamazepine;
- cholestyramine;
- griseofulvin;
- oral contraceptives;
- rifampicin;
- HIV protease inhibitors (e.g. ritonavir, nelfinavir);
- thiazide diuretics;
- St. John's Wort/Hypericum perforatum;
- Inducers of CYP2C9, CYP2C19 or CYP3A4 may diminish the anticoagulant effect of nicoumalone. Vitamin E and corticosteroids (e.g. methylprednisolone, prednisone) may diminish the anticoagulant effect of coumarin derivatives. Unpredictable effect on anticoagulation, including both increase and decrease in anticoagulant activity have been reported with the following drugs: protease inhibitors (e.g. indinavir, nelfinavir, ritonavir, saquinavir).
Effects of nicoumalone on other drugs:
During concomitant treatment with hydantoin derivatives (such as phenytoin), the serum hydantoin concentration may rise. Artiflo may potentiate the hypoglycaemic effect of sulphonylurea derivatives e.g. glibenclamide, glimepiride. Patients being treated with Artiflo (especially those suffering from hepatic dysfunction) should limit their alcohol intake, since it is not possible to predict the severity of any drug interactions, nor identify any early signs of such interactions. Cranberry juice should be avoided in patients receiving Artiflo due to a theoretical risk of enhanced anti-coagulation. Increased medical supervision and INR monitoring should be considered for any patient receiving Artiflo and regularly drinking cranberry juice. It is not known whether other cranberry products, such as capsules or concentrates, might also interact with Artiflo. Therefore, similar caution should be observed with these products.
Fertility, pregnancy and lactation
Pregnancy
Artiflo, like other coumarin derivatives, may be associated with congenital malformations of the embryo, therefore Artiflo is contra-indicated for use in pregnancy. Women of child-bearing potential should take contraceptive measures during treatment with Artiflo.
Breastfeeding
Nicoumalone passes into the breast milk, but in quantities so small that no undesirable effects on the infant are to be expected. However, as a precaution, the infant should be given 1mg vitamin K1 per week as a prophylactic measure. The decision to breast-feed should be carefully considered and may include coagulation tests and vitamin K status evaluation in infants before advising women to breast-feed. Women who are breast-feeding and treated with Artiflo should be carefully monitored to ensure that recommended PT/INR values are not exceeded.
Fertility
There are no data available on the use of Artiflo and its effect on fertility in humans.
Effects on ability to drive and use machines
Artiflo has no influence on the ability to drive and use machines. However, patients should be advised to keep their anticoagulant card with them.
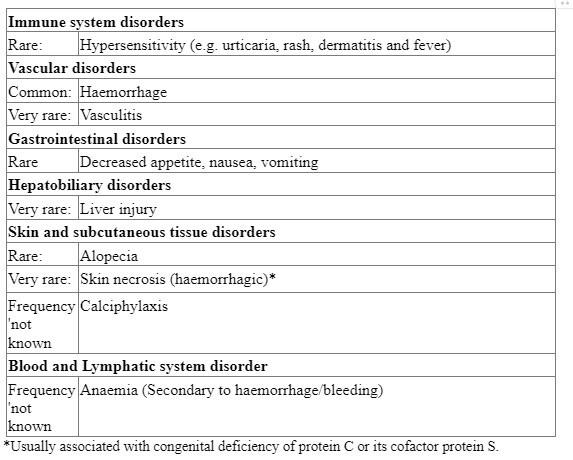
Undesirable effects
Undesirable effects are ranked under headings of frequency, the most frequent first, using the following convention: Very common (≥ 1/10); common (≥ 1/100, < 1/10); uncommon (≥ 1/1000, < 1/100); rare (≥ 1/10,000, < 1/1000); very rare (< 1/10,000), including isolated reports. Haemorrhage, in various organs, is the most common side-effect associated with Artiflo; its occurrence is related to the dosage of the drug, the patient's age and the nature of the underlying disease. Fatalities have been reported. Possible sites of haemorrhage include the gastro-intestinal tract, brain, urogenital tract, uterus, liver, gall bladder and the eye. If haemorrhage occurs in a patient with a thromboplastin time within the therapeutic range, diagnosis of their condition must be clarified.
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via email to: medico@zuventus.com By reporting side effects, you can help provide more information on the safety of this medicine.
Overdose
Clinical manifestations of overdosage are unlikely with large single doses, but more likely following prolonged use of daily doses exceeding those required therapeutically.
Hospital referral is recommended for any amount of Artiflo taken above the therapeutic dose.
Symptoms:
The onset and severity of the symptoms are dependent on the individual's sensitivity to oral anticoagulants, the severity of the overdose and the duration of treatment. Haemorrhage is the prominent feature of an overdose and may occur within 1 to 5 days after ingestion. Nose-bleeds, haematemesis, haemoptysis, gastro-intestinal haemorrhage, vaginal bleeding, haematuria (with renal colic), cutaneous haemorrhages, gingival bleeding, haematomata, and bleeding into the joints or menorrhagia may be experienced.
Further symptoms include tachycardia, hypotension, peripheral circulatory disorders due to loss of blood, nausea, vomiting, diarrhoea and abdominal pains. Laboratory tests will show an extremely low Quick value (or high PT/INR value), pronounced prolongation of the recalcification time or thromboplastin time and disturbed gamma-carboxylation of factors II, VII, IX and X.
Treatment:
The necessity or desirability of the treatment by gastric lavage in addition to the activated charcoal and cholestyramine administration is controversial. The benefits of these treatments should be balanced against the risk of bleeding in each patient. Emergency and supportive
measures:
In emergency situations of severe haemorrhage, clotting factors can be returned to normal by administering fresh whole blood or fresh frozen plasma, complex concentrate or recombinant factor VIIa supplemented with vitamin K1.
Antidote:
Vitamin K1 (phytomenadione) may antagonise the inhibitory effect of Artiflo on hepatic gamma-carboxylation of the vitamin K-dependent coagulation factors within 3 to 5 hours. In cases of clinically insignificant haemorrhages, such as a brief nose-bleed or small isolated haematomas, a temporary reduction or omission of the dose of Artiflo is often sufficient. In cases of moderate to severe haemorrhage, Vitamin K1 can be given orally.
Doses of Vitamin K1 in excess of 5mg can cause resistance to further anticoagulant therapy for several days. If an anticoagulant is required, heparin may be used temporarily, although oral anticoagulant therapy should be resumed at the same time and heparin withdrawn once the therapeutic range has been reached.
In the case of life-threatening haemorrhage, intravenous transfusions of fresh frozen plasma or whole blood, complex concentrate or recombinant factor VIIa supplemented with vitamin K1 can abolish the effects of Artiflo. Artiflo should be resumed when INR is in target range in case of moderate to severe haemorrhage.
Pharmacological properties
Pharmacodynamic properties
Pharmacotherapeutic group: Antithrombotic, vitamin K antagonists. ATC code: B01AA07
Mechanism of action
Nicoumalone is a coumarin derivative and functions as vitamin K antagonist. Vitamin K antagonists produce their anticoagulant effect by inhibition of the vitamin K-epoxide-reductase with a subsequent reduction of the gamma-carboxylation of certain glutamic acid molecules which are located at several sites near the terminal end both of coagulation factors II (prothrombin), VII, IX, and X and of protein C or its cofactor protein S. Pharmacodynamic effects This gamma-carboxylation has a significant bearing on interaction of the aforementioned coagulation factors with Calcium ions. Without this reaction, blood clotting cannot be initiated. Clinical efficacy and safety Depending on the initial dosage, Artiflo prolongs the thromboplastin time within approximately 36 to 72 hours. Following withdrawal of Artiflo, the thromboplastin time usually reverts to normal after a few days.
Pharmacokinetic properties
Absorption
Nicoumalone, is a racemic mixture of the optical R (+) and S (-) enantiomers. Following oral administration, Artiflo is rapidly absorbed; at least 60% of the administered dose is systemically available. Peak plasma concentrations are achieved within 1 to 3 hours after a single dose of 10 mg and AUC values are proportional to the size of the dose over a dosage range of 8 to 16 mg.
No correlation between plasma concentrations of nicoumalone and the apparent prothombin levels can be established, due to the variation of plasma drug concentrations between patients.
Distribution
Over 98% of nicoumalone is protein-bound, mainly to albumin. The calculated apparent volume of distribution is 0.16-0.18 L/kg for the R(+) enantiomer and 0.22-0.34 L/kg for the S(-) enantiomer.
Biotransformation
Nicoumalone is extensively metabolised, 6- and 7-hydroxylation of both enantiomers of Nicoumalone are the major metabolites and the cytochrome P450 2C9 is the major catalyst for the formation of these four metabolites. Other enzymes involved in the metabolism of (R)-nicoumalone are CYP1A2 and CYP2C19. By reduction of the keto group two different carbinol metabolites are formed. Reduction of the nitro group results in an amino metabolite. None of these metabolites contribute to the anticoagulant activity of the parent drug in man, but they are all active in an animal model. CYP2C9-related genetic variability accounts for 14% of the inter-individual variability in nicoumalone pharmacodynamics response.
Elimination
The elimination half-life of nicoumalone from the plasma is 8 to 11 hours. The apparent plasma clearance amounts to 3.65 L/h after oral administration. The total plasma clearance of the (+) enantiomer of nicoumalone, which possesses significantly higher anticoagulant activity, is much lower than that of the S(-) enantiomer. 29% is excreted in the faeces and 60% in the urine, with less than 0.2% of the dose renally excreted being unchanged.
Elderly
Plasma drug concentrations are generally higher in patients of 70 years or over when compared with younger patients, after the same dose.
Renal impairment
No clinical pharmacokinetic information of Nicoumalone in renal impairment is available. Based on the urinary excretion of Nicoumalone, the possibility of accumulation of metabolites in impaired renal function cannot be excluded. Therefore, usage of Nicoumalone is contraindicated in patient with severe renal impairment and caution should be exercised in patients with mild to moderate renal impairment.
Hepatic impairment
No clinical pharmacokinetic information of nicoumalone in hepatic impairment is available. Based on the metabolism of nicoumalone, and possible reduced enzyme activities, CYP2C9, CYP1A2 and CYP3A4, clearance is likely to be reduced. Therefore, usage of nicoumalone is contraindicated in patients with severe hepatic impairment and caution should be exercised in patients with mild to moderate hepatic impairment.
Ethnicity
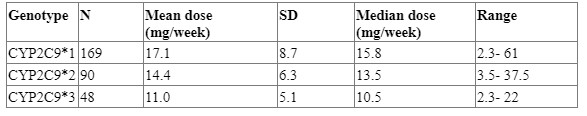
CYP2C9 enzyme systems are polymorphically expressed and the frequency of these in population differs. In Caucasians, occurrence of CYP2C9*2 and CYP2C9*3 frequencies are 12 and 8%, respectively. Patients with one or more of these variant CYP2C9 alleles have decreased clearance of S- Nicoumalone. In African patients, CYP2C9*2 and CYP2C9*3 occur at much lower allele frequencies 1-4% and 0.5-2.3%, respectively compared to Caucasians. Japanese population had lower allelic frequencies of 0.1% and 1-6% for CYP2C9*2 and CYP2C9*3, respectively]. The maintenance dose of nicoumalone differs based on the genotype. Detailed information of mean and median maintenance dose based on CYP2C9 genotype is given in the table below:
Table 1 CYP2C9 genotype and maintenance dose of Nicoumalone
Nonclinical properties
Toxicity
After a single (acute) oral and/or intravenous dose, Nicoumalone showed a low degree of toxicity in mice, rats, and rabbits. In dogs, high acute oral toxicity was seen. In repeated-dose studies, the liver is suggested to be the main target organ in the toxicity of coumarin derivatives including Nicoumalone. The administration of these substances at excessive pharmacological doses can cause haemorrhages.
Reproduction toxicity, teratogenicity
No reproductive toxicity studies were performed with Nicoumalone. However, placental and transplacental interference with vitamin K dependent coagulation factors may give rise to embryonic or foetal anomalies and neonatal haemorrhages both in animals and in humans.
Mutagenicity
From investigations on bacterial and mammalian cell systems in vitro, including a DNA repair assay on rat hepatocytes, it can be concluded that Nicoumalone and/or its metabolites did not exert any mutagenic effects. An in vitro study on human lymphocytes has shown some mild mutagenic activity at a concentration of Nicoumalone, 500 to 1000 times higher than concentrations determined in human plasma after medication with Nicoumalone.
Carcinogenicity
No lifetime-exposure studies were carried out in animals with Nicoumalone. Coumarin, induced an increase in the incidence of lung and benign liver tumours in mice, and liver and benign kidney tumours in rats. Liver tumours in rats and lung tumours in mice are understood to be associated with species-specific metabolic pathways in these species. Hepatoxicity of coumarin and its derivatives in the rat is understood to be associated with enzyme induction and the metabolic pathway of coumarin and/or its metabolites peculiar to this rodent species. Renal tumours observed in male mice are considered to be a species-specific effect.
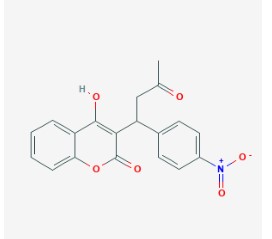
Description
Nicoumalone is a 4-hydroxycoumarin derivative with anticoagulant activity. As a vitamin K antagonist, Nicoumalone inhibits vitamin K epoxide reductase, thereby inhibiting the reduction of vitamin K and the availability of vitamin KH2. This prevents gamma carboxylation of glutamic acid residues near the N-terminals of the vitamin K-dependent clotting factors, including factor II, VII, IX, and X and anticoagulant proteins C and S. This prevents their activity and thus thrombin formation. Compared to other coumarin derivatives, Nicoumalone has a short half-life.
Chemical Structure
IUPAC Name: 4-hydroxy-3-[1-(4-nitrophenyl)-3-oxobutyl]chromen-2-one Molecular Formula: C19H15NO6 Molecular Weight: 353.3 g/mol
Pharmaceutical particulars
Incompatibilities
None stated.
Shelf-life
24 months
Packaging information
10 blister strips of 10 tablets each
Storage and handing instructions
Store protected from light & moisture at a temperature not exceeding 300C. Keep out of reach of children.
Patient Counselling Information
- Nicoumalone can cause major (including hemorrhagic and hypovolemic shock) or fatal bleeding. Risk factors for bleeding include
- high intensity of anticoagulation (INR >4.0)
- age ≥ 65, history of highly variable INRs
- history of gastrointestinal bleeding
- hypertension, cerebrovascular disease
- serious heart disease
- anemia, malignancy, trauma
- renal insufficiency, concomitant drugs
- Regular monitoring of INR should be performed on all treated patients.
- Those at high risk of bleeding may benefit from more frequent INR monitoring, careful dose adjustment to desired INR, and a shorter duration of therapy.
- In paediatric and elderly patients (≥65 years), caution and more frequent monitoring of PT/INR is recommended