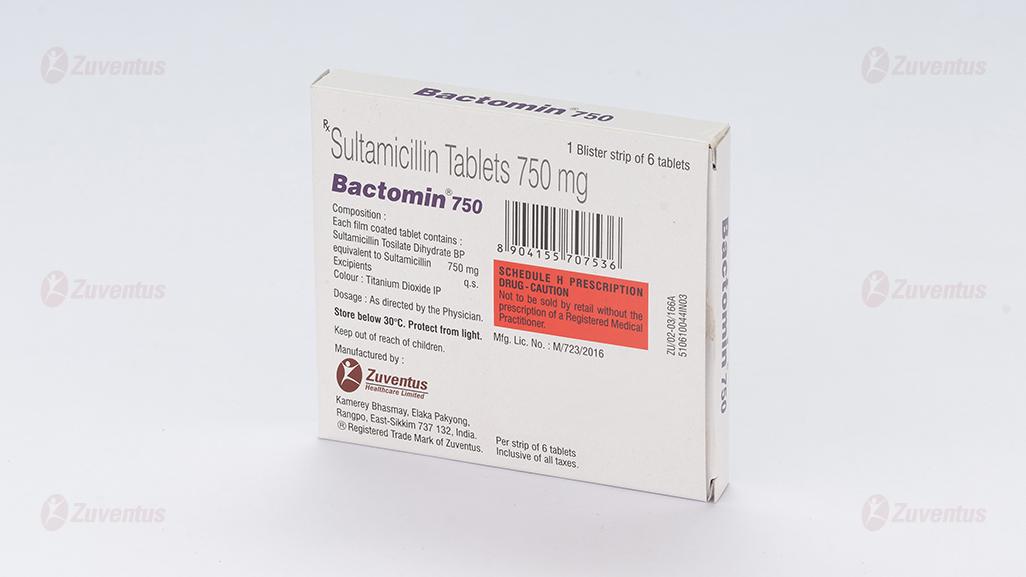
Bactomin 750 Tablets
Therapy Area
Anti Infective
1.0 Generic name
Sultamicillin Tablets
2.0 Qualitative and quantitative composition
Bactomin 375
Each film coated tablet contains:
Sultamicillin Tosilate Dihydrate BP
equivalent to Sultamicillin………………………………………. 375 mg
Bactomin 750
Each film coated tablet contains:
Sultamicillin Tosilate Dihydrate BP
equivalent to Sultamicillin………………………………………. 750 mg
3.0 Dosage form and strength
Tablet 375 mg/750 mg
4.0 Clinical particulars
4.1 Therapeutic indication
- Intra-abdominal infections
- Obstetrics and gynaecological infections
- Skin and soft tissue infections
- Bone and joint infections
- Upper and lower respiratory tract infections
- ENT infections
- Urinary tract infections
- Gonorrhoea
4.2 Posology and method of administration
The recommended dose of sultamicillin in adults (including elderly patients) is 375-750 mg orally twice daily.
In both adults and children, treatment is usually continued until 48 hours after pyrexia and other abnormal signs have resolved. Treatment is normally given for 5-14 days but the treatment period may be extended if necessary.
In the treatment of uncomplicated gonorrhea, sultamicillin can be given as a single oral dose of 2.25 g (six 375 mg tablets or three 750 mg tablets). Concomitant probenecid 1.0 g should be administered in order to prolong plasma concentrations of sulbactam and ampicillin.
Cases of gonorrhea with a suspected lesion of syphilis should have dark field examinations before receiving sultamicillin and monthly serological tests for a minimum of four months.
It is recommended that there be at least 10 days’ treatment for any infection caused by hemolytic streptococci to prevent the occurrence of acute rheumatic fever or glomerulonephritis.
Use in Children and Infants
The dosage for most infections in children weighing less than 30 kg is sultamicillin 25-50 mg/kg/day orally in two divided doses, depending on the severity of the infection and the physician's judgment. For children weighing 30 kg or more, the usual adult dose should be given.
Use in Patients with Renal Impairment
In patients with severe impairment of renal function (creatinine clearance ≤30 mL/min), the elimination kinetics of sulbactam and ampicillin are similarly affected and hence the plasma ratio of one to the other will remain constant. The dose of sultamicillin in such patients should be administered less frequently in accordance with usual practice for ampicillin.
4.3 Contraindications
Individuals with a history of an allergic reaction to any of the penicillins.
4.4 Special warnings and precautions for use
Serious and occasionally fatal hypersensitivity (anaphylactic) reactions have been reported in patients on penicillin therapy including sultamicillin. These reactions are more apt to occur in individuals with a history of penicillin hypersensitivity and/or hypersensitivity reactions to multiple allergens. There have been reports of individuals with a history of penicillin hypersensitivity who have experienced severe reactions when treated with cephalosporins. Before therapy with penicillin, careful inquiry should be made concerning previous hypersensitivity reactions to penicillins, cephalosporins, and other allergens. If an allergic reaction occurs, the drug should be discontinued and the appropriate therapy instituted.
Serious anaphylactic reactions require immediate emergency treatment with adrenaline. Oxygen, intravenous steroids, and airway management, including intubation, should be administered as indicated.
Severe skin reactions, such as toxic epidermal necrolysis (TEN), Stevens-Johnson syndrome (SJS), dermatitis exfoliative, and erythema multiforme have been reported in patients on ampicillin/sulbactam therapy. If a severe skin reaction occurs, use of the product should be discontinued and appropriate therapy should be initiated. As with any antibiotic preparation, constant observation for signs of overgrowth of non-susceptible organisms, including fungi, is essential. Should super-infection occur, the drug should be discontinued and/or appropriate therapy instituted.
Clostridium difficile-associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including sultamicillin, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon, leading to overgrowth of C. difficile.
C. difficile produces toxins A and B, which contribute to the development of CDAD. Hypertoxin-producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
Drug induced liver injury such as cholestatic hepatitis and jaundice have been associated with the use of ampicillin/sulbactam. Patients should be advised to contact their doctor if signs and symptoms of hepatic disease develop.
Since infectious mononucleosis is viral in origin, ampicillin should not be used in the treatment. A high percentage of patients with mononucleosis who receive ampicillin develop a skin rash. It is advisable to check periodically for organ system dysfunction during prolonged therapy; this includes renal, hepatic and hematopoietic systems. The principal route of excretion of sulbactam and ampicillin following oral administration of sultamicillin is via the urine. Because renal function is not fully developed in neonates, this should be considered when using sultamicillin in neonates.
4.5 Drugs interactions
Allopurinol
The concurrent administration of allopurinol and ampicillin increases substantially the incidence of rashes in patients receiving both drugs as compared to patients receiving ampicillin alone.
Anticoagulants
Penicillins can produce alterations in platelet aggregation and coagulation tests. These effects may be additive with anticoagulants.
Bacteriostatic drugs (chloramphenicol, erythromycin, sulfonamides and tetracyclines)
Bacteriostatic drugs may interfere with the bactericidal effect of penicillins; it is best to avoid concurrent therapy.
Estrogen-containing oral contraceptives
There have been case reports of reduced oral contraceptive effectiveness in women taking ampicillin, resulting in unplanned pregnancy. Although the association is weak, patients should be given the option to use an alternate or additional method of contraception while taking ampicillin.
Methotrexate
Concurrent use with penicillins has resulted in decreased clearance of methotrexate and a corresponding increase in methotrexate toxicity. Patients should be closely monitored. Leucovorin dosages may need to be increased and administered for longer periods of time.
Probenecid
Probenecid decreases renal tubular secretion of ampicillin and sulbactam when used concurrently; this effect results in increased and prolonged serum concentrations, prolonged elimination half-life, and increased risk of toxicity.
4.6 Use in special populations
Pregnancy
Animal reproduction studies have revealed no evidence of impaired fertility or harm to the fetus due to sultamicillin. Sulbactam and ampicillin cross the placental barrier. However, safety for use in human pregnancy has not been established. Therefore, sultamicillin should be used during pregnancy only if the potential benefits outweigh the potential risk.
Lactation
The use of sultamicillin during lactation is not recommended. Low concentrations of ampicillin and sulbactam are excreted in the milk. This should be considered as the neonate may be exposed, particularly since renal function is not fully developed in neonates.
4.7 Effects on ability to drive and use machines
No studies on the effect on the ability to drive and use machines have been performed.
4.8 Undesirable effects
Sultamicillin is generally well tolerated. The majority of side effects observed were of mild or moderate severity and were normally tolerated with continued treatment.
Infections and Infestations: Pseudomembranous colitis, Candida infection.
Blood and Lymphatic System Disorders: Thrombocytopenia.
Immune System Disorders: Anaphylactic shock, Anaphylactic reaction, Kounis syndrome, Hypersensitivity.
Nervous System Disorders: Dizziness, Somnolence, Sedation, Headache.
Respiratory, Thoracic and Mediastinal Disorders: Dyspnea.
Gastrointestinal Disorders: Enterocolitis, Melena, Diarrhea, Vomiting, Abdominal pain, Dyspepsia, Nausea, Stomatitis, Dysgeusia, Tongue discoloration.
Hepatobiliary Disorders: Jaundice, Hepatic function abnormal
Skin and Subcutaneous Tissue Disorders: Toxic epidermal necrolysis, Stevens-Johnson syndrome, Erythema multiforme, Angioedema, Urticaria, Dermatitis, Rash, Pruritus.
Musculoskeletal and Connective Tissue Disorders: Arthralgia.
General Disorders and Administration Site Conditions: Fatigue, Malaise.
Investigations: Alanine aminotransferase increased, Aspartate aminotransferase increased
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via email to: medico@zuventus.com
Website: https://www.zuventus.com/drug-safety-reporting
By reporting side effects, you can help provide more information on the safety of this medicine.
4.9 Overdose
Limited information is available on the acute toxicity of ampicillin sodium and sulbactam sodium in humans. Overdosage of the drug would be expected to produce manifestations that are principally extensions of the adverse reactions reported with the drug. The fact that high cerebrospinal fluid (CSF) concentrations of beta-lactam antibiotics may cause neurologic effects, including seizures, should be considered. Because ampicillin and sulbactam are both removed from the circulation by hemodialysis, these procedures may enhance elimination of the drug from the body if overdosage occurs in patients with impaired renal function.
5.0 Pharmacological properties
5.1 Mechanism of Action / Pharmacodynamic Properties
Biochemical studies with cell-free bacterial systems have shown sulbactam to be an irreversible inhibitor of most important beta-lactamases that occur in penicillin-resistant organisms. While sulbactam antibacterial activity is mainly limited to Neisseriaceae, the potential for sulbactam sodium in preventing the destruction of penicillins and cephalosporins by resistant organisms was confirmed in whole-organism studies using resistant strains, in which sulbactam sodium exhibited marked synergistic effects with penicillins and cephalosporins. Since sulbactam also binds to some penicillin-binding proteins, some sensitive strains are rendered more susceptible to the combination than to the beta-lactam antibiotic alone. The bactericidal component of this product is ampicillin, which, like benzyl penicillin, acts against sensitive organisms during the stage of active multiplication by the inhibition of biosynthesis of cell wall mucopeptide.
Sultamicillin is effective against a wide range of gram-positive and gram-negative bacteria including: Staphylococcus aureus and Staphylococcus epidermidis (including penicillin-resistant and some methicillin-resistant strains); Streptococcus pneumoniae, Streptococcus faecalis and other Streptococcus species; Haemophilus influenzae and Haemophilus parainfluenzae (both beta-lactamase-positive and -negative strains); Moraxella catarrhalis; anaerobes including Bacteroides fragilis and related species; Escherichia coli; Klebsiella species; Proteus species (both indole-positive and indole-negative); Enterobacter species; Morganella morganii; Citrobacter species; Neisseria meningitidis and Neisseria gonorrhoeae.
5.2 Pharmacokinetic properties
Following oral administration in humans, sultamicillin is hydrolyzed during absorption to provide sulbactam and ampicillin in a 1:1 molar ratio in the systemic circulation. The bioavailability of an oral dose is 80% of an equal intravenous dose of sulbactam and ampicillin. Administration following food does not affect the systemic bioavailability of sultamicillin. Peak serum levels of ampicillin, following administration of sultamicillin, are approximately twice those of an equal dose of oral ampicillin. Elimination half-lives are approximately 0.75 and 1 hour for sulbactam and ampicillin, respectively, in healthy volunteers, with 50%-75% of each agent being excreted unchanged in the urine. Elimination half-lives are increased in the elderly and in patients with renal dysfunction. Probenecid decreases the renal tubular secretion of both ampicillin and sulbactam. Concurrent use of probenecid with sultamicillin results in increased and prolonged blood levels of ampicillin and sulbactam.
6.0 Nonclinical properties
While reversible glycogenosis was observed in laboratory animals, this phenomenon was dose- and time-dependent and is not expected to develop at the therapeutic doses and corresponding plasma levels attained during the relatively short periods of combined ampicillin/sulbactam therapy in humans. Long-term studies in animals have not been performed to evaluate the carcinogenic potential. The individual components of sultamicillin (ampicillin/sulbactam) tested negative for mutagenicity. Reproduction studies have been performed in mice and rats at doses in excess of the human dose and have revealed no evidence of impaired fertility or harm to the fetus due to sultamicillin.
7.0 Description
Sultamicillin is a double ester in which Ampicillin and the beta-lactamase inhibitor sulbactam are linked via a methylene group.
Chemical name: Oxymethylpenicillinate Sulphone ester of Ampicillin
Molecular weight: 594.7
8.0 Pharmaceutical particulars
8.1 Incompatibilities
Not applicable
8.2 Shelf-life
8.3 Packaging information
8.4 Storage and handing instructions
Store in a cool & dry place. Protect from light.
Keep out of reach of children.
9.0 Patient Counselling Information
- Your doctor has prescribed Bactomin Tablet to cure your infection and improve your symptoms.
- Do not skip any doses and finish the full course of treatment even if you feel better. Stopping it early may make the infection to come back and harder to treat.
- It can be taken with or without food or as directed by your doctor.
- Diarrhea may occur as a side effect but should stop when your course is complete. Inform your doctor if it doesn't stop or if you find blood in your stools.
- Discontinue Bactomin Tablet and inform your doctor immediately if you get a rash, itchy skin, swelling of face and mouth, or have difficulty in breathing.
12.0 Date of revision
16.09.2022
About Leaflet
Please read this leaflet carefully before you start using this medicine because it contains important information for you.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet.
What is in this leaflet
1. What Bactomin is and what it is used for
2. What you need to know before you use Bactomin
3. How to use Bactomin
4. Possible side effects
5. How to store Bactomin
6. Contents of the pack and other information
1. What Bactomin is and what it is used for
Bactomin contains the active substance sultamicillin, which is a combination of ampicillin and sulbactam. It is used to treat various infections caused by bacteria, including:
- Intra-abdominal infections
- Obstetric and gynecological infections
- Skin and soft tissue infections
- Bone and joint infections
- Upper and lower respiratory tract infections
- ENT (ear, nose, and throat) infections
- Urinary tract infections
- Gonorrhea
2. What you need to know before you take Bactomin
Do not take Bactomin if:
- You are allergic to sultamicillin, ampicillin, or any other penicillin antibiotics.
- You have had an allergic reaction to cephalosporins or other beta-lactam antibiotics.
Warnings and precautions:
- Serious allergic reactions, including anaphylaxis, have been reported. Inform your doctor if you have a history of allergies.
- Severe skin reactions, such as Stevens-Johnson syndrome, have been reported. Discontinue use and seek medical attention if you develop a rash.
- Clostridium difficile-associated diarrhea (CDAD) has been reported. Contact your doctor if you experience severe diarrhea.
- Inform your doctor if you have liver or kidney problems.
Other medicines and Bactomin:
- Inform your doctor if you are taking allopurinol, anticoagulants, bacteriostatic drugs, oral contraceptives, methotrexate, or probenecid.
Pregnancy and breastfeeding:
- Use during pregnancy only if the potential benefits outweigh the risks.
- Not recommended during breastfeeding as it can pass into breast milk.
Driving and using machines:
- No studies have been performed on the effects on the ability to drive and use machines.
3. How to take Bactomin
Always use Bactomin exactly as your doctor has told you. You should check with your doctor or pharmacist if you are not sure.
Dosage:
- Adults: 375-750 mg orally twice daily.
- Children (under 30 kg): 25-50 mg/kg/day in two divided doses.
- Children (30 kg or more): Usual adult dose.
- For uncomplicated gonorrhea: Single dose of 2.25 g (six 375 mg tablets or three 750 mg tablets) with 1.0 g probenecid.
Method of administration:
- Take the tablets with or without food as directed by your doctor.
- Continue the full course of treatment even if you feel better.
If you use more Bactomin than you should
Tell your doctor if you accidentally use more than you were told.
If you forget to use Bactomin
If you forget to take at the right time, use it as soon as you remember, then carry on as before. Do not take a double dose to make up for a forgotten dose.
If you stop using Bactomin
Do not stop your treatment even if you feel better unless told to do so by your doctor. If you have any further questions on the use of this product, ask your doctor or pharmacist.
4. Possible side effects
Common side effects:
- Diarrhea, nausea, vomiting, abdominal pain
- Rash, itching
Serious side effects:
- Severe allergic reactions (anaphylaxis)
- Severe skin reactions (Stevens-Johnson syndrome)
- Clostridium difficile-associated diarrhea (CDAD)
- Liver problems (jaundice)
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly: Website: www.zuventus.com in and click the tab “Safety Reporting” located on the top end of the home page. Website link: https://www.zuventus.com/drug-safety-reporting. By reporting side effects, you can help provide more information on the safety of this medicine. You can also report the side effect with the help of your treating physician.
5. How to store Bactomin
- Keep this medicine out of the sight and reach of children.
- Do not store above 25°C. Do not freeze.
- Do not use this medicine after the expiry date which is stated on the label and carton after EXP.
- The expiry date refers to the last day of that month.
Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help protect the environment.
6. Contents of the pack and other information
What Bactomin contains:
- Active substance: Sultamicillin Tosilate Dihydrate equivalent to Sultamicillin 375 mg or 750 mg.