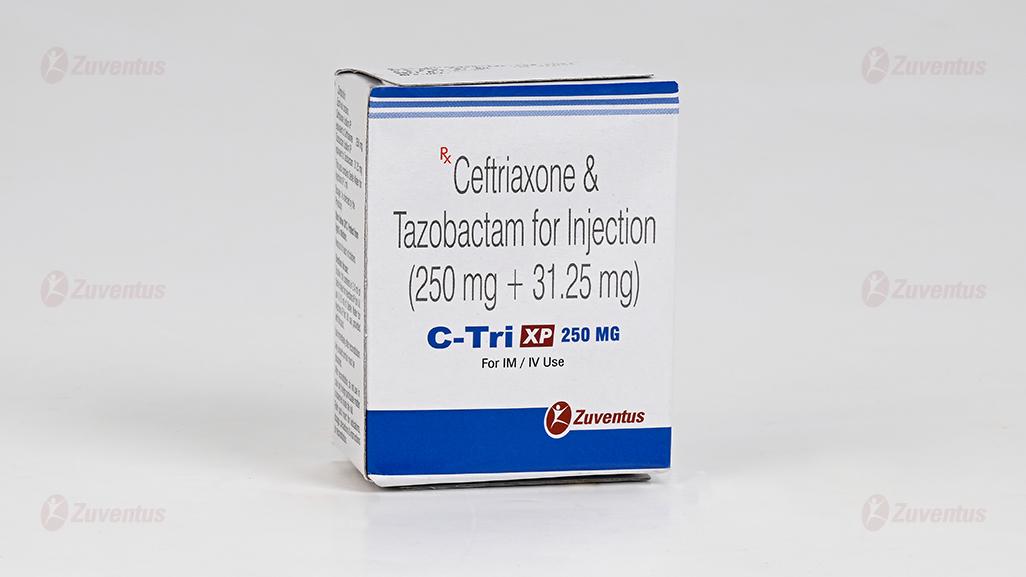
C Tri XP 250 mg
Therapy Area
Anti Infective
1.0 Generic name
Ceftriaxone & Tazobactam for Injection
2.0 Qualitative and quantitative composition
C-Tri XP KID 125 mg
Each vial contains :
Ceftriaxone Sodium IP equivalent to Ceftriaxone 125 mg
Tazobactam Sodium IP equivalent to Tazobactam 15.625 mg
This pack contains Sterile Water for Injections IP 5 ml.
C-Tri XP 250 mg
Each vial contains :
Ceftriaxone Sodium IP equivalent to Ceftriaxone 250 mg
Tazobactam Sodium IP equivalent to Tazobactam 31.25 mg
This pack contains Sterile Water for Injections IP 5 ml.
C-Tri XP 500 mg
Each vial contains :
Ceftriaxone Sodium IP equivalent to Ceftriaxone 500 mg
Tazobactam Sodium IP equivalent to Tazobactam 62.5 mg
This pack contains Sterile Water for Injections IP 5 ml.
C-Tri XP 1 g
Each vial contains :
Ceftriaxone Sodium IP equivalent to Ceftriaxone 1.0 g
Tazobactam Sodium IP equivalent to Tazobactam 125 mg
This pack contains Sterile Water for Injections IP 10 ml.
3.0 Dosage form and strength
Powder for solution for infusion.
125 mg / 250 mg / 500 mg / 1 gm
4.0 Clinical particulars
4.1 Therapeutic indication
- Bacterial meningitis
- Community acquired pneumonia
- Hospital acquired pneumonia
- Acute otitis media
- Intra-abdominal infections
- Complicated urinary tract infections (including pyelonephritis)
- Infections of bones and joints
- Complicated skin and soft tissue infections
- Gonorrhoea
- Syphilis
- Bacterial endocarditis
- Surgical prophylaxis
4.2 Posology and method of administration
C-Tri XP Injection to be administered by deep intramuscular (I.M.) injection, slow intravenous (I.V.) injection, or as a slow I.V. infusion, after reconstitution with sterile water for injection (SWFI).
Dosage Recommendations in Adults
Usual Recommended Dose : 1.125 g to 2.25 g of C-Tri XP Injection (1 g / 2 g ceftriaxone + 125 mg / 250 mg tazobactam) per day given once a day or in two equally divided doses every 12 hours. The total daily dose of ceftriaxone should not exceed 4 grams. Tazobactam can be given up to 2 grams per day.
For Uncomplicated Gonococcal Infections : A single dose of 562.5 mg of C-Tri XP Injection (500 mg ceftriaxone + 62.5 mg tazobactam) to be administered by I.M. route. For Preoperative Use (Surgical Prophylaxis) : A single dose of 1.125 g of C-Tri XP Injection (1g ceftriaxone + 125 mg tazobactam) to be administered I.V. 30 minutes to 2 hours before surgery. The usual duration of therapy is 4 to 14 days. In complicated infections, longer therapy may be required.
Or, as prescribed by the physician.
Dosage in Adult Patients with Renal Impairment and Hepatic Dysfunction.
In patients with both hepatic dysfunction and significant renal disease, caution should be exercised and the ceftriaxone dosage should not exceed 2 gram daily. Tazobactam should be used with care in patients with renal impairment or in hemodialysis patients. The I.V. dose and administration interval should be adjusted to the degree of renal function impairment.
Dosage Recommendations in Pediatric Patients
For children with bodyweight above 50 kg or age over 12 years, the usual adult dosage should be administered. Although, ceftriaxone can be administered in neonates and infants, the safety and efficacy of this combination product (ceftriaxone + tazobactam injection) has not been established in children below 2 years of age. Thus, C-Tri XP Injection is recommended only in children above 2 years of age.
Following doses in children are expressed in terms of ceftriaxone content of the formulation. Usual Recommended Dosage : 50 to 75 mg/kg/day, given in divided doses every 12 hours. The total daily dose of ceftriaxone should not exceed 2 grams. In children, tazobactam can be given up to 12.5 mg/kg body weight per dose.
Treatment of Meningitis : The initial therapeutic dose should be 100 mg/kg body weight. Thereafter, daily dose of 100 mg/kg may be administered once a day or in equally divided doses every 12 hours. The total daily dose of ceftriaxone should not exceed 4 grams. The usual duration of therapy is 7 to 14 days depending on the type and severity of infection. Or, as prescribed by the physician.
Pharmaceutical Precautions
Ceftriaxone-containing injection should not be mixed with other drugs in infusion bottle since compatibility has not been established. Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration, whenever solution and container permit.
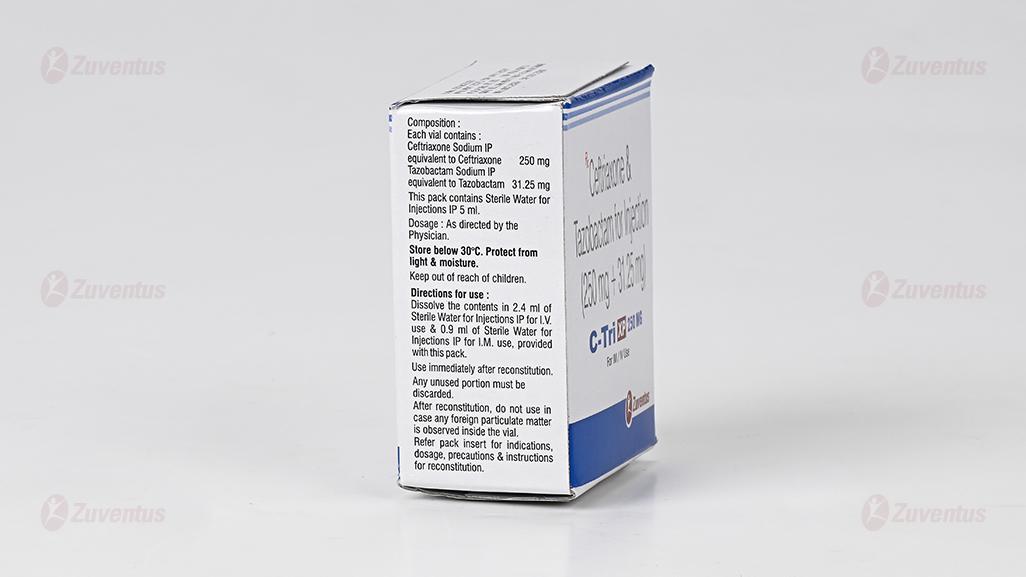
Directions for reconstitution and dilution for use
Intramuscular injection : Contents of one vial should be dissolved in 0.45 ml of Sterile Water for Injections IP for C-Tri XP-KID 125 mg of injection, 0.9 ml of Sterile Water for Injections IP for C-Tri XP-250 mg injection, 1.8 ml of Sterile Water for Injections IP for C-Tri XP-500 mg injection and 3.6 ml of Sterile Water for Injections IP for C-Tri XP-1 g injection. The solution should be administered by deep intramuscular injection. Doses greater than 1 g (of Ceftriaxaone) should be divided and injected at more than one site.
Intravenous injection : Contents of one vial should be dissolved in 1.2 ml of Sterile Water for Injections IP for C-Tri XP-KID 125 mg of injection, 2.4 ml of Sterile Water for Injections IP for C-Tri XP-250 mg injection, 4.8 ml of Sterile Water for Injections IP for C-Tri XP-500 mg injection and 9.6 ml of Sterile Water for Injections IP for C-Tri XP-1 g injection. The solution should be administered over at least 2-4 minutes, directly into the vein or via the tubing of an intravenous infusion.
Incompatibility / Interaction with Calcium-Containing Products
Do not use diluents containing calcium, such as Ringer's solution or Hartmann's solution, to reconstitute or to further dilute a reconstituted vial for I.V. administration because a precipitate can form. Precipitation of ceftriaxone-calcium can also occur when ceftriaxone is mixed with calcium-containing solutions in the same I.V. administration line.
Ceftriaxone with tazobactam must not be administered simultaneously with calcium-containing I.V. solutions, including continuous calcium-containing infusions such as parenteral nutrition.
4.3 Contraindications
- In patients with known hypersensitivity to ceftriaxone,cephalosporin class of antibiotics, or to tazobactam or to any component of the formulation.
- In hyperbilirubinemic neonates/preterm newborns : Ceftriaxone can displace bilirubin from its binding to serum albumin, leading to a risk of bilirubin encephalopathy in these patients.
- Premature neonates : Ceftriaxone is contraindicated in premature neonates up to a postmenstrual age of 41 weeks (gestational age + chronological age).
- In neonates (≤ 28 days) if they require (or are expected to require) treatment with calcium-containing I.V. solutions, including continuous calcium-containing infusions such as parenteral nutrition because of the risk of precipitation of ceftriaxone-calcium.
- Intravenous administration of ceftriaxone solutions containing lidocaine is contraindicated.
4.4 Special warnings and precautions
Test Dose
Before therapy with ceftriaxone and tazobactam injection is instituted, a test dose is recommended to ascertain possibility of hypersensitivity to ingredients of injection. Serious acute hypersensitivity reactions may require the use of subcutaneous epinephrine and other emergency measures.
Hypersensitivity
Before initiation of therapy, careful inquiry should be made to determine whether the patient has had previous hypersensitivity reactions to cephalosporins, penicillins and other beta-lactam agents or other drugs. As with all beta-lactam antibacterial agents, serious and occasionally fatal hypersensitivity reactions (i.e., anaphylaxis) have been reported. In case of severe hypersensitivity reactions, treatment with ceftriaxone must be discontinued immediately and adequate emergency measures must be initiated.
Clostridium Difficile-Associated Diarrhea (CDAD)
CDAD has been reported with use of nearly all antibacterial agents, including ceftriaxone, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile. If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
Hemolytic Anemia
An immune mediated hemolytic anemia has been observed in patients receiving cephalosporin class of antibacterial drugs including ceftriaxone. Severe cases of hemolytic anemia, including fatalities, have been reported during treatment in both adults and children. If a patient develops anemia while on ceftriaxone, the diagnosis of a cephalosporin associated anemia should be considered and ceftriaxone stopped until the etiology is determined.
Development of Drug-Resistant Bacteria
Prescribing ceftriaxone in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria. Prolonged use of ceftriaxone may result in overgrowth of nonsusceptible organisms. Careful observation of the patient is essential. If superinfection occurs during therapy, appropriate measures should be taken.
Pancreatitis
Cases of pancreatitis, possibly secondary to biliary obstruction, have been reported in patients treated with ceftriaxone. Most patients presented with risk factors for biliary stasis and biliary sludge (preceding major therapy, severe illness, and total parenteral nutrition). A cofactor role of ceftriaxone-related biliary precipitation cannot be ruled out.
Urolithiasis and Post-Renal Acute Renal Failure
Ceftriaxone-calcium precipitates in the urinary tract have been observed in patients receiving ceftriaxone. The probability of such precipitates appears to be greatest in pediatric patients. Patients may be asymptomatic or may develop symptoms of urolithiasis, and ureteral obstruction and post-renal acute renal failure. The condition appears to be reversible upon discontinuation of ceftriaxone and institution of appropriate management. Ensure adequate hydration in patients receiving ceftriaxone. Discontinue ceftriaxone in patients who develop signs and symptoms suggestive of urolithiasis, oliguria or renal failure and/or the sonographic findings.
Gallbladder Pseudolithiasis
Ceftriaxone-calcium precipitates in the gallbladder have been observed in patients receiving ceftriaxone. The probability of such precipitates appears to be greatest in pediatric patients. Patients may be asymptomatic or may develop symptoms of gallbladder disease. The condition appears to be reversible upon discontinuation of ceftriaxone and institution of conservative management. Discontinue ceftriaxone sodium in patients who develop signs and symptoms suggestive of gallbladder disease and/or the sonographic findings.
Effect on Prothrombin Time
Alterations in prothrombin times have occurred in patients treated with ceftriaxone. Monitor prothrombin time during ceftriaxone treatment in patients with impaired vitamin K synthesis or low vitamin K stores (e.g., chronic hepatic disease and malnutrition). Vitamin K administration (10 mg weekly) may be necessary if the prothrombin time is prolonged before or during therapy.
Altered Laboratory Tests
Positive direct Coombs' test and galactosemia test, false-positive test for urinary glucose and elevated lactate dehydrogenase (LDH).
4.5 Drug interactions
Ceftriaxone
Amsacrine, Vancomycin, Fluconazole, and Aminoglycosides : Ceftriaxone is incompatible with these drugs.
Oral Contraceptives : Ceftriaxone may adversely affect the efficacy of oral hormonal contraceptives. Consequently, it is advisable to use supplementary (non-hormonal) contraceptive measures during treatment and in the month following treatment.
Chloramphenicol : Caution is advised if concurrent administration of ceftriaxone with chloramphenicol is proposed.
Vitamin K Antagonist : Concomitant use of ceftriaxone with vitamin K antagonists may increase the risk of bleeding. Coagulation parameters should be monitored frequently, and the dose of the anticoagulant adjusted accordingly, both during and after treatment with ceftriaxone.
Tazobactam
Probenecid : When probenecid administered concomitantly with tazobactam, it prolongs the half-life of tazobactam by 71%. This is because probenecid inhibits tubular renal secretion of tazobactam. Probenecid should not be co-administered with tazobactam unless the benefit outweighs the risk.
4.6 Use in special populations
Pregnancy
Animal studies have revealed no evidence of impaired fertility or harm to the fetus. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, C-Tri XP Injection should be used during pregnancy only if clearly needed.
Lactation
Low quantities of both ceftriaxone and tazobactam are excreted in human milk. Therefore, caution should be exercised when C-Tri XP Injection is administered to a nursing woman. Women who are breast-feeding should be treated only if the expected benefit outweighs the possible risks to the woman and child.
Pediatric patients
Safety and effectiveness of ceftriaxone has been established in pediatric patients. In vitro studies have shown that ceftriaxone, like some other cephalosporins, can displace bilirubin from serum albumin. Thus, ceftriaxone-containing preparations should not be administered to hyperbilirubinemic children. Safety and efficacy of C-Tri XP Injection has not been established in children below 2 years of age.
Geriatric patients
Dosage adjustments are not necessary for geriatric patients with ceftriaxone dosages up to 2 grams per day provided there is no severe renal and hepatic impairment.
4.7 Effects on the ability to drive and use machines
During treatment with ceftriaxone and tazobactam combination, undesirable effects such as dizziness, headache, and convulsions may occur, which may influence the ability to drive and
use machines. If affected by such events, patients should not drive or operate machinery.
4.8 Undesirable effects
Ceftriaxone-containing preparations are generally well tolerated. In clinical trials, the following adverse reactions were observed (related to ceftriaxone therapy or of uncertain etiology).
Local Reactions : Injection site pain, induration, tenderness, phlebitis, warmth, tightness. Hypersensitivity : Rash, pruritus, fever or chills.
Infections and Infestations : Genital fungal infection.
Hematologic : Eosinophilia, thrombocytosis, leukopenia. Less frequently reported were anemia, hemolytic anemia, neutropenia, lymphopenia, thrombocytopenia and prolongation of the prothrombin time.
Blood and Lymphatic Disorders : Granulocytopenia, coagulopathy.
Gastrointestinal : Diarrhea/loose stools, nausea, vomiting, dysgeusia, pseudomembranous colitis.
Hepatic : Elevations of aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase, and bilirubin.
Renal : Elevations of the blood urea nitrogen (BUN), creatinine and the presence of casts in the urine.
Central Nervous System : Headache, dizziness.
Genitourinary : Moniliasis, vaginitis.
Dermatologic : Exanthema, allergic dermatitis, urticaria, edema; acute generalized exanthematous pustulosis (AGEP) and isolated cases of severe cutaneous adverse reactions (erythema multiforme, Stevens-Johnson syndrome or Lyell's syndrome / toxic epidermal necrolysis) have been reported.
Miscellaneous : Diaphoresis, flushing, increased blood creatinine.
Other rarely observed adverse reactions (< 0.1%) include abdominal pain, agranulocytosis, allergic pneumonitis, anaphylaxis, basophilia, biliary lithiasis, bronchospasm, colitis, dyspepsia, epistaxis, flatulence, gallbladder sludge, glycosuria, hematuria, jaundice, leukocytosis, lymphocytosis, monocytosis, nephrolithiasis, palpitations, decrease in the prothrombin time, renal precipitations, seizures, and serum sickness.
Reporting of side effects
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via email to : medico@zuventus.com
Website : https://www.zuventus.co.in/drug-safety-reporting
By reporting side effects, you can help provide more information on the safety of this medicine.
4.9 Overdose
In the case of overdose nausea, vomiting, and diarrhea can occur. There is no specific antidote. Treatment should be supportive and symptomatic according the patient's clinical presentation.
5.0 Pharmacological properties
5.1 Mechanism of action
Ceftriaxone
Ceftriaxone is a third generation cephalosporin class of beta-lactam antibiotic. Ceftriaxone inhibits bacterial cell wall synthesis and produces bactericidal effect. Ceftriaxone has activity in the presence of some beta-lactamases, both penicillinases and cephalosporinases, of Gramnegative and Gram-positive bacteria.
Tazobactam
Beta-lactamases are the enzymes produced by certain bacteria to develop resistant to antibiotics. Tazobactam, a beta-lactam structurally related to penicillins, is an inhibitor of many beta-lactamases, which commonly cause resistance to penicillins and cephalosporins. Tazobactam has good inhibitory activity against the clinically important plasmid mediated beta-lactamases most frequently responsible for transferred drug resistance.
Rationale of the combination
Ceftriaxone is a third generation semi-synthetic parenteral cephalosporin that has excellent activity against variety of gram -ve organisms and some gram +ve organisms like Streptococcus pneumoniae, Staphylococcus aureus, H.influenzae, Neisseria meningitides and members of Enterobacteriaceae. Ceftriaxone is indicated in number of community and hospital acquired infections caused by the susceptible organisms both in adults and in children including neonates.
Tazobactam is penicillanic acid sulfone derivative with beta-lactamase inhibitory properties, having good affinity for a variety of both plasmid mediated and chromosomal beta lactamases produced by gram +ve and gram –ve bacteria which are originally sensitive to Ceftriaxone. Therefore, it enhances the activity of penicillins and cephalosporins against many resistant strains of bacteria. It is regarded as more potent than other β-lactamase inhibitors (like sulbactam).
Clinical role of Ceftriaxone can be compromised due to increasing proportion of extended spectrum β-lactamase (ESBL) producing bacteria which exhibit resistance to Ceftriaxone. To treat such infections Ceftriaxone can be combined with a beta lactamases inhibitor of better efficacy like Tazobactam. The combination of Ceftriaxone and Tazobactam will be effective not only against the beta lactamase producing organisms but also against the originally Ceftriaxone-susceptible bacteria.
5.2 Pharmacodynamic properties
The combination of ceftriaxone and tazobactam is active against wide variety of beta-lactamase producing gram-positive and gram-negative bacteria. In addition, it demonstrates synergistic activity (reduction in MICs of combination therapy versus ceftriaxone alone) in a variety of organisms which are sensitive to ceftriaxone.
C-Tri XP Injection has been shown to be active against most isolates of the following bacteria, both in vitro and in clinical infections :
Gram-negative Bacteria
Acinetobacter calcoaceticus, Enterobacter aerogenes, Enterobacter cloacae, Escherichia coli, Haemophilus influenzae, Haemophilus parainfluenzae, Klebsiella oxytoca, Klebsiella pneumoniae, Moraxella catarrhalis, Morganella morganii, Neisseria gonorrhoeae, Neisseria meningitidis, Proteus mirabilis, Proteus vulgaris, Pseudomonas aeruginosa, Serratia marcescens
Gram-positive Bacteria
Staphylococcus aureus, Staphylococcus epidermidis, Streptococcus pneumoniae, Streptococcus pyogenes, Viridans group streptococci
Anaerobic Bacteria
Bacteroides fragilis, Clostridium species, Peptostreptococcus species
The following in vitro data are available, but their clinical significance is unknown. At least 90% of the following microorganisms exhibit an in vitro minimum inhibitory concentration (MIC) less than or equal to the susceptible breakpoint for ceftriaxone. However, the efficacy of ceftriaxone in treating clinical infections due to these microorganisms has not been established in adequate and well-controlled clinical trials.
Gram-negative Bacteria
Citrobacter diversus, Citrobacter freundii, Providencia species (including Providencia rettgeri), Salmonella species (including Salmonella typhi), Shigella species
Gram-positive Bacteria
Streptococcus agalactiae
Anaerobic Bacteria
Porphyromonas (Bacteroides) melaninogenicus, Prevotella (Bacteroides) bivius
5.3 Pharmacokinetics
Ceftriaxone
Absorption : Following intramuscular injection, mean peak plasma ceftriaxone levels are approximately half those observed after intravenous administration of an equivalent dose. The maximum plasma concentration after a single intramuscular dose of 1 gram is about 81 mg/l and is reached in 2 to 3 hours after administration. The area under the plasma concentrationtime curve after intramuscular administration is equivalent to that after intravenous administration of an equivalent dose.
After intravenous bolus administration of ceftriaxone 500 mg and 1 g, mean peak plasma ceftriaxone (Cmax) levels are approximately 120 and 200 mg/l respectively. After intravenous infusion of ceftriaxone 500 mg, 1 g and 2 g, the plasma ceftriaxone levels are approximately 80, 150 and 250 mg/l respectively. An 8 to 15 % increase in Cmax is seen on repeated administration; steady state is reached in most cases within 48 to 72 hours depending on the route of administration.
Distribution : The volume of distribution of ceftriaxone is 7 to 12 litre. Ceftriaxone is reversibly bound to albumin. Plasma protein binding is about 95 % at plasma concentrations below 100 mg/l. Binding is saturable and the bound portion decreases with rising concentration (up to 85 % at a plasma concentration of 300 mg/l).
Metabolism : Ceftriaxone is not metabolized systemically; but is converted to inactive metabolites by the gut flora.
Elimination : Plasma clearance of total ceftriaxone (bound and unbound) is 10 to 22 ml/min. Renal clearance is 5 to 12 ml/min. 50 to 60 % of ceftriaxone is excreted unchanged in the urine, primarily by glomerular filtration, while 40 to 50 % is excreted unchanged in the bile. The elimination half-life of total ceftriaxone in adults is about 8 hours.
Tazobactam
Peak plasma concentration is attained immediately after completion of an I.V. infusion. Plasma protein binding of tazobactam is approximately 23%. Tazobactam is widely distributed in tissues and body fluids including intestinal mucosa, gall bladder, lung and bile.
Approximately 20% of a dose of tazobactam is metabolized to a single metabolite that has been found to be microbiologically inactive. Tazobactam is eliminated by the kidney via glomerular filtration and tubular secretion. Tazobactam and its metabolite are eliminated primarily by renal excretion, with 80% of the dose appearing as unchanged drug and the remainder of the dose appearing as the metabolite. In healthy subjects, plasma elimination half-life of tazobactam range from 0.7 to 1.2 hours following single or multiple doses.
6.0 Nonclinical properties
6.1 Animal Toxicology or Pharmacology
Ceftriaxone
LD50 values after administration of ceftriaxone by intravenous route were in mice 1840 mg/kg, in rat 2240 mg/kg, and in rabbit 240 mg/kg. LD50 value reported after administration of ceftriaxone by oral route in mice and rats was >10,000 mg/kg. In a 2-week intravenous administration study, groups of eight male Füllinsdorf rats were administered 0, 25 or 60 mg/kg/day of ceftriaxone. Body weight gain was slightly depressed by 9.2 and 20.1% in the 25 and 60 mg/kg/day groups respectively. The average weight of the thyroid glands was increased in the treated groups by 11 to 14% in comparison to the control animals. A 50% reduction in plasma bilirubin in the treated rats was reported along with a decrease in the number of leucocytes. 11 Genetic toxicology tests included the Ames test, a micronucleus test and a test for chromosomal aberrations in human lymphocytes cultured in vitro with ceftriaxone. Ceftriaxone showed no potential for mutagenic activity in these studies. Carcinogenicity studies on ceftriaxone were not conducted. Reproductive studies have been performed in mice and rats at doses up to 20 times the usual human dose and have no evidence of embryotoxicity, fetotoxicity or teratogenicity. In primates, no embryotoxicity or teratogenicity was demonstrated at a dose approximately 3 times the human dose. Ceftriaxone produced no impairment of fertility when given intravenously to rats at daily doses up to 586 mg/kg/day, approximately 20 times the recommended clinical dose of 2 g/day.
Tazobactam
In an embryo-fetal study in rats, tazobactam administered at doses up 3000 mg/kg/day (approximately 19 times the recommended human dose based on body surface area comparison) did not produce maternal toxicity, or fetal toxicity or teratogenicity. Reproductive toxicity : In males, tazobactam had no effect on epididymal and testes weight or mating and fertility indexes. In females, tazobactam did not produce changes in the female estrus cycle length, days in cohabitation, mating index, fertility index, fetal body weight, or fetal gender ratio. In female rats that underwent caesarean section, the number of surviving offspring was reduced to a non-significant degree with the high-dose (640 mg/kg/day) of tazobactam. In high-dose females that were allowed to proceed to delivery without caesarean section, the number of implantations was significantly decreased, and this finding was accompanied by a significant increase in the number of still births and a non-significant decrease in the number of surviving offspring compared to control values. Tazobactam was shown to be negative for mutagenicity or clastogenesis in an Ames assay, a chromosomal aberration assay, and an in vivo micronucleus assay.
7.0 Description
C-Tri XP is a combination of Ceftriaxone, a semi - synthetic third generation broad spectrum cephalosporin antibiotic along with a β- lactamase inhibitor Tazobactam. Tazobactam sodium, a derivative of the penicillin nucleus, is a penicillanic acid sulfone.
Ceftriaxone
Ceftriaxone is a beta-lactam, third-generation cephalosporin antibiotic with bactericidal activity.
Molecular Weight : 554.6g/mol.
Molecular Formula : C18H18N8O7S3.
Chemical Name : (6R,7R)-7-[[(2Z)-2-(2-amino-1,3-thiazol-4-yl)-2-methoxyimino acetyl]amino]- 3-[(2-methyl-5,6-dioxo-1H-1,2,4-triazin-3-yl)sulfanylmethyl]-8-oxo-5-thia-1- azabicyclo[4.2.0]oct-2-ene-2-carboxylic acid.
Tazobactam
Tazobactam sodium, a derivative of the penicillin nucleus, is a penicillanic acid sulfone. Tazobactam is a β-lactamase inhibitor given in combination with β-lactam antibiotics to inhibit β-lactamase, an enzyme produced by bacteria that destroys antibiotic activity.
Molecular Weight : 322.28g/mol.
Molecular Formula : C10H11N4NaO5S.
Chemical Name : Sodium (2S,3S,5R)-3-methyl-7-oxo-3-(1H-1,2,3-triazol-1-ylmethyl)-4- thia-1- azabicyclo[3.2.0] heptane-2-carboxylate-4,4-dioxide.
8.0 Pharmaceutical particulars
8.1 Incompatibilities
8.2 Shelf-life
Refer to the pack.
8.3 Packaging information
C-Tri XP KID 125 mg : A vial of 140.625 mg with SWFI IP 5 ml.
C-Tri XP 250 mg : A vial of 281.25 mg with SWFI IP 5 ml.
C-Tri XP 500 mg : A vial of 562.5 mg with SWFI IP 5 ml.
C-Tri XP 1 g : A vial of 1.125 g with SWFI IP 10 ml.
8.4 Storage and handling instructions
Store below 30°C. Protect from light & moisture.
Keep out of reach of children. After reconstitution, do not use in case any foreign particulate matter is observed inside the vial.
9.0 Patient counselling information
Instruct patient to store medication as advised and not to expose the vial to moisture or direct light.
The medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may decrease the effectiveness of therapy and increase the likelihood that bacteria will develop antimicrobial resistance.
Diarrhea is a common problem caused by antibiotics which usually ends when the antibiotic is discontinued. Sometimes after starting treatment with antibiotics, patients can develop watery and bloody stools even as late as two months after the last dose of the antibiotic. If this occurs, instruct patients to contact their physician immediately.
Instruct patient not to freeze the reconstituted solution and use it immediately after the preparation. Unused portion of solution, if any, should be discarded.
12.0 Date of revision
13 August 2024