Dapaformin 500 Tablet
Therapy Area
Anti-diabetic
1.0 Generic name
Dapagliflozin & Metformin Hydrochloride Extended Release Tablets
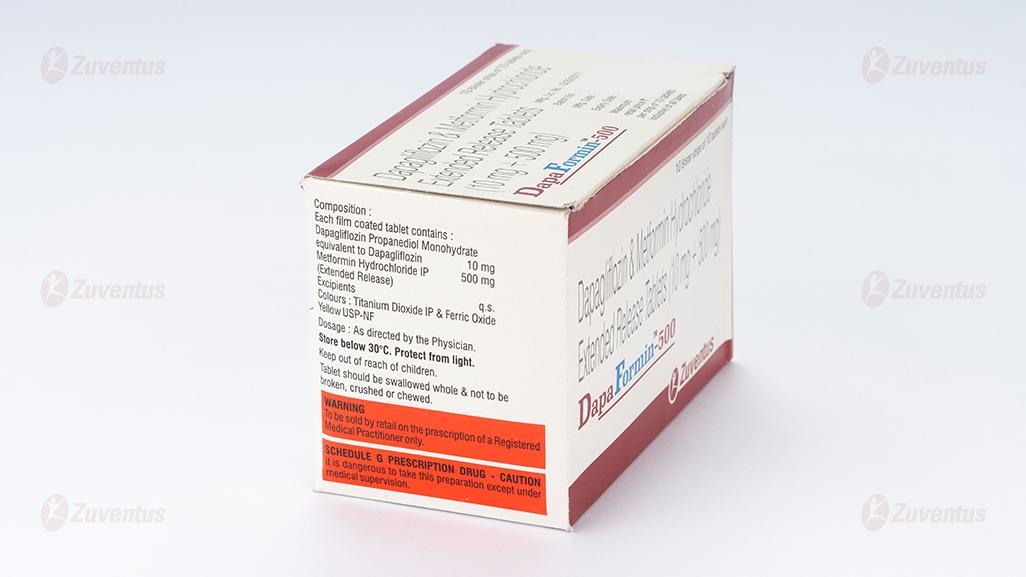
2.0 Qualitative and quantitative composition
DapaFormin-500
Each film coated tablet contains :
Dapagliflozin Propanediol Monohydrate
equivalent to Dapagliflozin 10 mg
Metformin Hydrochloride IP 500 mg
(Extended Release)
Excipients q.s Colours : Titanium Dioxide IP & Ferric Oxide Yellow USP-NF
DapaFormin-1000
Each film coated tablet contains :
Dapagliflozin Propanediol Monohydrate
equivalent to Dapagliflozin 10 mg
Metformin Hydrochloride IP 1000 mg
(Extended Release)
Excipients q.s
Colours : Titanium Dioxide IP & Ferric Oxide Yellow USP-NF
3.0 Dosage form and strength
Film coated tablet
4.0 Clinical particulars
4.1 Therapeutic indication
It is indicated as an adjunct to diet and exercise to improve glycaemic control in adults with type 2 diabetes mellitus when treatment with both Dapagliflozin and Metformin is appropriate.
4.2 Posology and method of administration
Dapagliflozin + Metformin ER tablet once daily in the morning with food or as directed by physician. Swallow Dapagliflozin Metformin ER tablets whole and never crush, cut, or chew
4.3 Contraindications
- Severe renal impairment (eGFR below 30 mL/min/1.73 m2 ), end stage renal disease or patients on dialysis
- History of a serious hypersensitivity reaction to dapagliflozin or hypersensitivity to metformin hydrochloride
- Acute or chronic metabolic acidosis, including diabetic ketoacidosis, with or without coma. Diabetic ketoacidosis should be treated with insulin
4.4 Special warnings and precautions for use
Lactic Acidosis
In Dapagliflozin + Metformin ER tablets a treated patient with a diagnosis or strong suspicion of lactic acidosis, prompt hemodialysis is recommended to correct the acidosis and remove accumulated metformin (metformin hydrochloride is dialyzable, with a clearance of up to 170 mL/min under good hemodynamic conditions). Hemodialysis has often resulted in reversal of symptoms and recovery. The postmarketing metformin-associated lactic acidosis cases primarily occurred in patients with significant renal impairment. The risk of metformin accumulation and metformin-associated lactic acidosis increases with the severity of renal impairment because metformin is substantially excreted by the kidney.
Hypotension
Dapagliflozin 2 causes intravascular volume contraction. Symptomatic hypotension can occur after initiating dapagliflozin, particularly in patients with impaired renal function (eGFR less than 60 mL/min/1.73 m ), elderly patients, or patients on loop diuretics. Before initiating Dapagliflozin + Metformin ER tablets in patients with one or more of these characteristics, volume status should be assessed and corrected. Monitor for signs and symptoms of hypotension after initiating therapy.
Ketoacidosis
Reports of ketoacidosis, a serious life-threatening condition requiring urgent hospitalization have been identified in postmarketing surveillance in patients with type 1 and type 2 diabetes mellitus taking sodium-glucose co transporter 2 (SGLT2) inhibitors, including dapagliflozin. Fatal cases of ketoacidosis have been reported in patients taking dapagliflozin. Dapagliflozin + Metformin ER tablet is not indicated for the treatment of patients with type 1diabetes mellitus
Acute Kidney Injury and Impairment in Renal Function
Dapagliflozin causes intravascular volume contraction and can cause renal impairment. There have been postmarketing reports of acute kidney injury, some requiring hospitalization and dialysis, in patients receiving dapagliflozin : some reports involved patients younger than 65 years of age. Before initiating Dapagliflozin + Metformin ER tablet, consider factors that may predispose patients to acute kidney injury including hypovolemia, chronic renal insufficiency, congestive heart failure, and concomitant medications (diuretics, ACE inhibitors, ARBs, NSAIDs). Consider temporarily discontinuing Dapagliflozin + Metformin ER tablet in any setting of reduced oral intake (such as acute illness or fasting) or fluid losses (gastrointestinal illness or excessive heat exposure); monitor patients for signs and symptoms of acute kidney injury. If acute kidney injury occurs, discontinue Dapagliflozin + Metformin ER tablet promptly and institute treatment.
4.5 Drugs interactions
Coadministration of multiple doses of dapagliflozin and metformin does not meaningfully alter the pharmacokinetics of either dapagliflozin or metformin in healthy subjects
No interaction studies have been performed for Dapaformin. The following statements reflect the information available on the individual active substances.
Dapagliflozin
Pharmacodynamic interactions
Diuretics
This medicinal product may add to the diuretic effect of thiazide and loop diuretics and may increase the risk of dehydration and hypotension.
Insulin and insulin secretagogues
Insulin and insulin secretagogues, such as sulphonylureas, cause hypoglycaemia. Therefore, a lower dose of insulin or an insulin secretagogue may be required to reduce the risk of hypoglycaemia when used in combination with dapagliflozin.
Pharmacokinetic interactions
The metabolism of dapagliflozin is primarily via glucuronide conjugation mediated by UDP-glucuronosyltransferase 1A9 (UGT1A9)
In vitro studies, dapagliflozin neither inhibited cytochrome P450 (CYP) 1A2, CYP2A6, CYP2B6, CYP2C8, CYP2C9, CYP2C19, CYP2D6, CYP3A4, nor induced CYP1A2, CYP2B6 or CYP3A4. Therefore, this medicinal product is not expected to alter the metabolic clearance of coadministered medicinal products that are metabolised by these enzymes.
Effect of other medicinal products on dapagliflozin Interaction studies conducted in healthy subjects, using mainly a single-dose design, suggest that the pharmacokinetics of dapagliflozin are not altered by pioglitazone, sitagliptin, glimepiride, voglibose, hydrochlorothiazide, bumetanide, valsartan, or simvastatin.
Following coadministration of dapagliflozin with rifampicin (an inducer of various active transporters and drug-metabolising enzymes) a 22% decrease in dapagliflozin systemic exposure (AUC) was observed, but with no clinically meaningful effect on 24-hour urinary glucose excretion. No dose adjustment is recommended. A clinically relevant effect with other inducers (e.g. carbamazepine, phenytoin, phenobarbital) is not expected. Following coadministration of dapagliflozin with mefenamic acid (an inhibitor of UGT1A9), a 55% increase in dapagliflozin systemic exposure was seen, but with no clinically meaningful effect on 24-hour urinary glucose excretion. No dose adjustment is recommended.
Effect of dapagliflozin on other medicinal products In interaction studies conducted in healthy subjects, using mainly a single-dose design, dapagliflozin did not alter the pharmacokinetics of pioglitazone, sitagliptin, glimepiride, hydrochlorothiazide, bumetanide, valsartan, digoxin (a P-gp substrate) or warfarin (S-warfarin, a CYP2C9 substrate), or the anti-coagulatory effects of warfarin as measured by INR. Combination of a single dose of dapagliflozin 20 mg and simvastatin (a CYP3A4 substrate) resulted in a 19% increase in AUC of simvastatin and 31% increase in AUC of simvastatin acid. The increase in simvastatin and simvastatin acid exposures are not considered clinically relevant.
Interference with 1,5-anhydroglucitol (1,5-AG) assay Monitoring glycaemic control with 1,5-AG assay is not recommended as measurements of 1,5-AG are unreliable in assessing glycaemic control in patients taking SGLT2 inhibitors. Use of alternative methods to monitor glycaemic control is advised.
Metformin
Concomitant use not recommended Cationic substances that are eliminated by renal tubular secretion (e.g. cimetidine) may interact with metformin by competing for common renal tubular transport systems. A study conducted in seven normal healthy volunteers showed that cimetidine, administered as 400 mg twice daily, increased metformin systemic exposure (AUC) by 50% and Cmax by 81%. Therefore, close monitoring of glycaemic control, dose adjustment within the recommended posology and changes in diabetic treatment should be considered when cationic medicinal products that are eliminated by renal tubular secretion are coadministered.
Alcohol
Alcohol intoxication is associated with an increased risk of lactic acidosis, particularly in the case of fasting, malnutrition or hepatic impairment due to the metformin active substance of this medicinal product. Consumption of alcohol and medicinal products containing alcohol should be avoided.
Iodinated contrast agents
Intravascular administration of iodinated contrast agents may lead to contrast induced nephropathy, resulting in metformin accumulation and increased risk of lactic acidosis. Xigduo must be discontinued prior to, or at the time of the imaging procedure and not restarted until at least 48 hours after, provided that renal function has been re-evaluated and found to be stable.
Combination requiring precautions for use
Glucocorticoids (given by systemic and local routes), beta-2 agonists, and diuretics have intrinsic hyperglycaemic activity. The patient should be informed and more frequent blood glucose monitoring perfomed, especially at the beginning of treatment with such medicinal products. If necessary, the dose of the glucose-lowering medicinal product should be adjusted during therapy with the other medicinal product and on its discontinuation.
Some medicinal products can adversely affect renal function which may increase the risk of lactic acidosis, e.g. NSAIDs, including selective cyclo-oxygenase (COX) II inhibitors, ACE inhibitors, angiotensin II receptor antagonists and diuretics, especially loop diuretics. When starting or using such products in combination with metformin, close monitoring of renal function is necessary
Insulin and insulin secretagogues
Insulin and insulin secretagogues, such as sulphonylureas, cause hypoglycaemia. Therefore, a lower dose of insulin or an insulin secretagogue may be required to reduce the risk of hypoglycaemia when used in combination with metformin
4.6 Use in special populations
Pregnancy
Based on animal data showing adverse renal effects, Dapagliflozin + Metformin ER tablet is not recommended during the second and third trimesters of pregnancy. Limited data with Dapagliflozin + Metformin ER tablet or dapagliflozin in pregnant women are not sufficient to determine drug-associated risk for major birth defects or miscarriage. Published studies with metformin use during pregnancy have not reported a clear association with metformin and major birth defect or miscarriage risk. There are risks to the mother and fetus associated with poorly controlled diabetes in pregnancy
Lactation
There is no information regarding the presence of Dapagliflozin + Metformin ER tablet or dapagliflozin in human milk, the effects on the breastfed infant, or the effects on milk production
Females and Males of Reproductive Potential Discuss the potential for unintended pregnancy with premenopausal women as therapy with metformin may result in ovulation in some anovulatory women.
Pediatric Use
Safety and effectiveness of Dapagliflozin + Metformin ER tablet in pediatric patients under 18 years of age have not been established.
Geriatric Use
No Dapagliflozin + Metformin ER tablet dosage change is recommended based on age. More frequent assessment of renal function is recommended in elderly patients.
Renal Impairment
In clinical studies dapagliflozin was associated with increases in serum creatinine and decreases in eGFR . Use of dapagliflozin is not recommended when eGFR is less than 45 mL/min/1.73 m and is contraindicated in patients with severe renal 2 impairment (eGFR less than 30 mL/min/1.73 m ) or ESRD.
Metformin is substantially excreted by the kidney, and the risk of metformin accumulation and lactic acidosis increases with the degree of renal impairment. Dapagliflozin + Metformin ER tablet is contraindicated in severe renal impairment, patients with 2 an estimated glomerular filtration rate (eGFR) below 30 mL/min/1.73 m
Hepatic Impairment
Use of metformin in patients with hepatic impairment has been associated with some cases of lactic acidosis. Dapagliflozin + Metformin ER tablet is not recommended in patients with hepatic impairment
4.7 Effects on ability to drive and use machines
Dapaformin has no or negligible influence on the ability to drive and use machines. Patients should be alerted to the risk of hypoglycaemia when this medicinal product is used in combination with other glucose-lowering medicinal products known to cause hypoglycaemia.
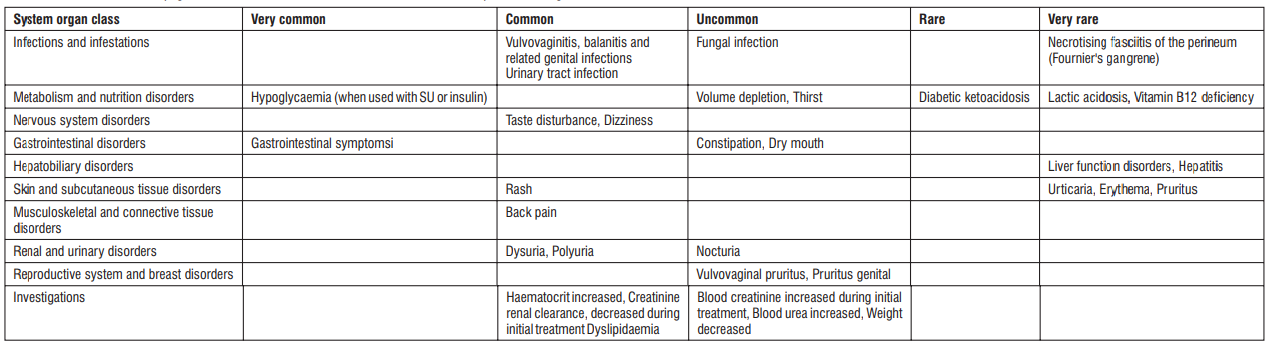
4.8 Undesirable effects
Dapaformin has been demonstrated to be bioequivalent with coadministered dapagliflozin and metformin. There have been no therapeutic clinical trials conducted with Dapaformin tablets.
Dapagliflozin plus metformin
Summary of the safety profile
In an analysis of 5 placebo-controlled dapagliflozin add-on to metformin studies, the safety results were similar to that of the pre-specified pooled analysis of 13 placebo-controlled dapagliflozin studies (see Dapagliflozin, Summary of the safety profile below). No additional adverse reactions were identified for the dapagliflozin plus metformin group compared with those reported for the individual components. In the separate dapagliflozin add-on to metformin pooled analysis, 623 subjects were treated with dapagliflozin 10 mg as add-on to metformin and 523 were treated with placebo plus metformin.
Dapagliflozin
Summary of the safety profile
In the clinical studies in type 2 diabetes, more than 15,000 patients have been treated with dapagliflozin.
The primary assessment of safety and tolerability was conducted in a pre-specified pooled analysis of 13 short-term (up to 24 weeks) placebo-controlled studies with 2,360 subjects treated with dapagliflozin 10 mg and 2,295 treated with placebo. In the dapagliflozin cardiovascular outcomes study (see section 5.1), 8,574 patients received dapagliflozin 10 mg and 8,569 received placebo for a median exposure time of 48 months. In total, there were 30,623 patient-years of exposure to dapagliflozin.
The most frequently reported adverse reactions across the clinical studies were genital infections.
Tabulated list of adverse reactions
The following adverse reactions have been identified in the placebo-controlled dapagliflozin plus metformin clinical studies, dapagliflozin clinical studies and metformin clinical studies and post-marketing experience. None were found to be doserelated. Adverse reactions listed below are classified according to frequency and system organ class. Frequency categories are defined according to the following convention: very common (≥ 1/10), common (≥ 1/100 to < 1/10), uncommon (≥ 1/1,000 to < 1/100), rare (≥ 1/10,000 to < 1/1,000), very rare (< 1/10,000), and not known (cannot be estimated from the available data).
Table : Adverse reactions in dapagliflozin and metformin immediate-release clinical trial and post-marketing data.
Description of selected adverse reactions
Dapagliflozin plus metformin
Hypoglycaemia
In studies with dapagliflozin in add-on combination with metformin, minor episodes of hypoglycaemia were reported at similar frequencies in the group treated with dapagliflozin 10 mg plus metformin (6.9%) and in the placebo plus metformin group (5.5%). No major events of hypoglycaemia were reported. Similar observations were made for the combination of dapagliflozin with metformin in drug-naive patients. In an add-on to metformin and a sulphonylurea study, up to 24 weeks, minor episodes of hypoglycaemia were reported in 12.8% of subjects who received dapagliflozin 10 mg plus metformin and a sulphonylurea and in 3.7% of subjects who received placebo plus metformin and a sulphonylurea. No major events of hypoglycaemia were reported.
Dapagliflozin
Vulvovaginitis, balanitis and related genital infections
n the 13-study safety pool, vulvovaginitis, balanitis and related genital infections were reported in 5.5% and 0.6% of subjects who received dapagliflozin 10 mg and placebo, respectively. Most infections were mild to moderate, and subjects responded to an initial course of standard treatment and rarely resulted in discontinuation from dapagliflozin treatment. These infections were more frequent in females (8.4% and 1.2% for dapagliflozin and placebo, respectively), and subjects with a prior history were more likely to have a recurrent infection.
In the dapagliflozin cardiovascular outcomes study, the number of patients with serious adverse events of genital infections were few and balanced : 2 patients in each of the dapagliflozin and placebo groups. Necrotising fasciitis of the perineum (Fournier's gangrene) Cases of Fournier's gangrene have been reported postmarketing in patients taking SGLT2 inhibitors, including dapagliflozin.
In the dapagliflozin cardiovascular outcomes study with 17,160 type 2 diabetes mellitus patients and a median exposure time of 48 months, a total of 6 cases of Fournier's gangrene were reported, one in the dapagliflozin-treated group and 5 in the placebo group.
Hypoglycaemia
The frequency of hypoglycaemia depended on the type of background therapy used in each study. For studies of dapagliflozin as add-on to metformin or as add-on to sitagliptin (with or without metformin), the frequency of minor episodes of hypoglycaemia was similar (< 5%) between treatment groups, including placebo up to 102 weeks of treatment. Across all studies, major events of hypoglycaemia were uncommon and comparable between the groups treated with dapagliflozin or placebo. In a study with add-on insulin therapy, higher rates of hypoglycaemia were observed. In an add-on to insulin study up to 104 weeks, episodes of major hypoglycaemia were reported in 0.5% and 1.0% of subjects in dapagliflozin 10 mg plus insulin at Weeks 24 and 104, respectively, and in 0.5% of subjects treated with placebo plus insulin groups at Weeks 24 and 104. At Weeks 24 and 104, minor episodes of hypoglycaemia were reported, respectively, in 40.3% and 53.1% of subjects who received dapagliflozin 10 mg plus insulin and in 34.0% and 41.6% of the subjects who received placebo plus insulin.
In the dapagliflozin cardiovascular outcomes study, no increased risk of major hypoglycaemia was observed with dapagliflozin therapy compared with placebo. Major events of hypoglycaemia were reported in 58 (0.7%) patients treated with dapagliflozin and 83 (1.0%) patients treated with placebo.
Volume depletion
In the 13-study safety pool, reactions suggestive of volume depletion (including, reports of dehydration, hypovolaemia or hypotension) were reported in 1.1% and 0.7% of subjects who received dapagliflozin 10 mg and placebo, respectively; serious reactions occurred in < 0.2% of subjects balanced between dapagliflozin 10 mg and placebo. In the dapagliflozin cardiovascular outcomes study, the numbers of patients with events suggestive of volume depletion were balanced between treatment groups: 213 (2.5%) and 207 (2.4%) in the dapagliflozin and placebo groups, respectively. Serious adverse events were reported in 81 (0.9%) and 70 (0.8%) in the dapagliflozin and placebo group, respectively. Events were generally balanced between treatment groups across subgroups of age, diuretic use, blood pressure and ACE-I/ARB 2 use. In patients with eGFR < 60 mL/min/1.73 m at baseline, there were 19 events of serious adverse events suggestive of volume depletion in the dapagliflozin group and 13 events in the placebo group. Diabetic ketoacidosis
In the dapagliflozin cardiovascular outcomes study, with a median exposure time of 48 months, events of DKA were reported in 27 patients in the dapagliflozin 10 mg group and 12 patients in the placebo group. The events occurred evenly distributed over the study period. Of the 27 patients with DKA events in the dapagliflozin group, 22 had concomitant insulin treatment at the time of the event. Precipitating factors for DKA were as expected in a type 2 diabetes mellitus population. Urinary tract infections
In the 13-study safety pool, urinary tract infections were more frequently reported for dapagliflozin compared with placebo (4.7% versus 3.5%, respectively). Most infections were mild to moderate, and subjects responded to an initial course of standard treatment and rarely resulted in discontinuation from dapagliflozin treatment. These infections were more frequent in females, and subjects with a prior history were more likely to have a recurrent infection. In the dapagliflozin cardiovascular outcomes study, serious events of urinary tract infections were reported less frequently for dapagliflozin 10 mg compared with placebo, 79 (0.9%) events versus 109 (1.3%) events, respectively. Increased creatinine
Adverse reactions related to increased creatinine were grouped (e.g. decreased renal creatinine clearance, renal impairment, increased blood creatinine and decreased glomerular filtration rate). This grouping of reactions was reported in 3.2% and 2 1.8% of patients who received dapagliflozin 10 mg and placebo, respectively. In patients with normal renal function or mild renal impairment (baseline eGFR ≥ 60 mL/min/1.73 m ) this grouping of reactions were reported in 1.3% and 0.8% of patients who 2 received dapagliflozin 10 mg and placebo, respectively. These reactions were more common in patients with baseline eGFR ≥ 30 and < 60 mL/min/1.73 m (18.5% dapagliflozin 10 mg vs 9.3% placebo). Further evaluation of patients who had renal-related adverse events showed that most had serum creatinine changes of ≤ 0.5 mg/dL from baseline. The increases in creatinine were generally transient during continuous treatment or reversible after discontinuation of treatment
In the dapagliflozin cardiovascular outcomes study, including elderly patients and patients with renal impairment (eGFR less than 60 mL/min/1.73 m ), eGFR decreased over time in both treatment groups. At 1 year, mean eGFR was slightly lower, and at 4 years, mean eGFR was slightly higher in the dapagliflozin group compared with the placebo group.
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse
reactions via email to: medico@zuventus.com
By reporting side effects, you can help provide more information on the safety of this medicine
4.9 Overdose
Dapagliflozin
There were no reports of overdose during the clinical development program for dapagliflozin. In the event of an overdose, contact the Poison Control Center. It is also reasonable to employ supportive measures as dictated by the patient’s clinical status. The removal of dapagliflozin by hemodialysis has not been studied.
Metformin hydrochloride
Overdose of metformin hydrochloride has occurred, including ingestion of amounts >50 grams. Hypoglycemia was reported in approximately 10% of cases, but no causal association with metformin hydrochloride has been established. Lactic acidosis has been reported in approximately 32% of metformin overdose cases. Metformin is dialyzable with a clearance of up to 170 mL/min under good hemodynamic conditions. Therefore, hemodialysis may be useful for removal of accumulated drug from patients in whom metformin overdosage is suspected.
5.0 Pharmacological properties
5.1 Mechanism of Action
Dapagliflozin + Metformin ER tablet combines two antihyperglycemic agents with complementary mechanisms of action to improve glycemic control in patients with type 2 diabetes: dapagliflozin, a sodiumglucose cotransporter 2 (SGLT2) inhibitor, and metformin hydrochloride, a biguanide. Dapagliflozin Sodium-glucose cotransporter 2 (SGLT2), expressed in the proximal renal tubules, is responsible for the majority of the reabsorption of filtered glucose from the tubular lumen. Dapagliflozin is an inhibitor of SGLT2. By inhibiting SGLT2, dapagliflozin reduces reabsorption of filtered glucose and lowers the renal threshold for glucose, and thereby increases urinary glucose excretion. Metformin hydrochloride Metformin improves glucose tolerance in patients with type 2 diabetes, lowering both basal and postprandial plasma glucose. Metfor min decreases hepatic glucose production, decreases intestinal absorption of glucose, and improves insulin sensitivity by increasing peripheral glucose uptake and utilization. Metformin does not produce hypoglycemia in either patients with type 2 diabetes or in healthy subjects, except in unusual circumstances, and does not cause hyperinsulinemia. With metformin therapy, insulin secretion remains unchanged while fasting insulin levels and day-long plasma insulin response may actually decrease.
5.2 Pharmacodynamic properties
Dapagliflozin
Increases in the amount of glucose excreted in the urine were observed in healthy subjects and in patients with type 2 diabetes mellitus following the administration of dapagliflozin Dapagliflozin doses of 5 or 10 mg per day in patients with type 2 diabetes mellitus for 12 weeks resulted in excretion of approximately 70 grams of glucose in the urine per day. A near maximum glucose excretion was observed at the dapagliflozin daily dose of 20 mg. This urinary glucose excretion with dapagliflozin also results in increases in urinary volume Dapagliflozin was not associated with clinically meaningful prolongation of QTc interval at daily doses up to 150 mg (15 times the recommended dose) in a study of healthy subjects. In addition, no clinically meaningful effect on QTc interval was observed following single doses of up to 500 mg (50 times the recommended dose) dapagliflozin in healthy subjects. Metformin In humans, independently of its action on glycaemia, metformin has favourable effects on lipid metabolism. This has been shown at therapeutic doses in controlled, medium-term or long-term clinical studies: metformin reduces total cholesterol, LDL cholesterol and triglyceride levels. In clinical studies, use of metformin was associated with either a stable body weight or modest weight loss.
5.3 Pharmacokinetic properties
Absorption
Dapagliflozin Following oral administration of dapagliflozin, the maximum plasma concentration (Cmax) is usually attained within 2 hours under fasting state. The Cmax and AUC values increase dose proportionally with increase in dapagliflozin dose in the therapeutic dose range. The absolute oral bioavailability of dapagliflozin following the administration of a 10 mg dose is 78%. Administration of dapagliflozin with a high-fat meal decreases its Cmax by up to 50% and prolongs Tmax by approximately 1 hour, but does not alter AUC as compared with the fasted state. These changes are not considered to be clinically meaningful and dapagliflozin can be administered with or without food. Metformin Hydrochloride The absolute bioavailability of a 500 mg metformin hydrochloride tablet given under fasting conditions is approximately 50 to 60%. Studies using single oral doses of metformin hydrochloride tablets 500 mg to 1,500 mg, and 850 mg to 2,550 mg, indicate that there is a lack of dose proportionality with increasing doses, which is due to decreased absorption rather than an alteration in elimination. Food decreases the extent of and slightly delays the absorption of metformin hydrochloride, as shown by approximately a 40% lower mean peak plasma concentration (Cmax), a 25% lower area under the plasma concentration versus time curve (AUC), and a 35 minute prolongation of the time to peak plasma concentration (Tmax) following administration of a single 850 mg tablet of metformin hydrochloride with food, compared to the same tablet strength administered under fasting conditions. The clinical relevance of these decreases is unknown.
Distribution
Dapagliflozin Dapagliflozin is approximately 91% protein bound. Protein binding is not altered in patients with renal or hepatic impairment. Metformin Hydrochloride The apparent volume of distribution (V/F) of metformin hydrochloride following single oral doses of 850 mg averaged 654 ± 358 litres. Metformin hydrochloride is negligibly bound to plasma proteins, in contrast to sulphonylureas, which are more than 90% protein bound. Metformin hydrochloride partitions into erythrocytes, most likely as a function of time. At usual clinical doses and dosing schedules of metformin hydrochloride, steady state plasma concentrations of metformin hydrochloride are reached within 24 to 48 hours and are generally<1 microgram/mL. During controlled clinical studies of metformin hydrochloride, maximum metformin hydrochloride plasma levels did not exceed 5 micrograms/mL, even at maximum doses
Biotransformation
Dapagliflozin The metabolism of dapagliflozin is primarily mediated by UGT1A9; CYP-mediated metabolism is a minor clearance pathway in humans. Dapagliflozin is extensively metabolized, primarily to yield dapagliflozin 3-O-glucuronide, which is an inactive metabolite. Dapagliflozin 3-O glucuronide accounted for 61% of a 50 mg [14C]-dapagliflozin dose and is the predominant drugrelated component in human plasma. Metformin Hydrochloride Metformin is excreted unchanged in the urine. No metabolites have been identified in humans.
Elimination
Dapagliflozin and related metabolites are primarily eliminated via the renal pathway. Following a single 50 mg dose of [14C]-dapagliflozin, 75% and 21% total radioactivity is excreted in urine and feces, respectively. In urine, less than 2% of the dose is excreted as parent drug. In feces, approximately 15% of the dose is excreted as parent drug. The mean plasma terminal half-life (t½) for dapagliflozin is approximately 12.9 hours following a single oral dose of dapagliflozin 10 mg.
Metformin Hydrochloride
Intravenous single-dose studies in normal subjects demonstrate that metformin hydrochloride is excreted unchanged in the urine and does not undergo hepatic metabolism (no metabolites have been identified in humans) nor biliary excretion. Renal clearance is approximately 3.5 times greater than creatinine clearance, which indicates that tubular secretion is the major route of elimination. Following oral administration, approximately 90% of the absorbed drug is eliminated via the renal route within the first 24 hours, with a plasma elimination half-life of approximately 6.2 hours. In blood, the elimination half-life is approximately 17.6 hours, suggesting that the erythrocyte mass may be a compartment of distribution.
6.0 Nonclinical properties
No known animal toxicology data
7.0 Description
Dapagliflozin, is a medication used to treat type 2 diabetes and, with certain restrictions, type 1 diabetes. It is also used to treat adults with heart failure with reduced ejection fraction to reduce the risk of cardiovascular death and hospitalization for heart failure.
The most common side effect in people with type 2 diabetes is hypoglycaemia, especially when used in combination with a sulphonylurea or insulin. The most common side effect in people with type 1 diabetes is genital infection, especially in women and a common side effect is diabetic ketoacidosis. It is of the gliflozin (SGLT2 inhibitor) class. Metformin, is the first-line medication for the treatment of type 2 diabetes, particularly in people who are overweight. It is also used in the treatment of polycystic ovary syndrome. It is not associated with weight gain. It is taken by mouth.
8.0 Pharmaceutical particulars
8.1 Incompatibilities
No incompatibility study have been found
8.2 Shelf-life
Refer on the pack
8.3 Packaging information
A blister strip of 10 tablets.
8.4 Storage and handing instructions
Store below 30°C. Protect from light.
Keep out of reach of children
9.0 Patient counselling information
Instruct patients to read the Medication Guide before starting treatment with and to reread it each time the prescription is renewed. Inform patients of the potential risks and benefits of Dapaformin and of alternative modes of therapy. Also inform patients about the importance of adherence to dietary instructions, regular physical activity, periodic blood glucose monitoring and HbA1c testing, recognition and management of hypoglycemia and hyperglycemia, and assessment of diabetes complications. Advise patients to seek medical advice promptly during periods of stress such as fever, trauma, infection, or surgery, as medication requirements may change. Inform patients that the incidence of hypoglycemia may be increased when Dapaformin is added to an insulin secretagogue (e.g., sulfonylurea) or insulin. Instruct patient to immediately inform her healthcare provider if she is pregnant or plans to become pregnant. Based on animal data, Dapaformin may cause fetal harm in the second and third trimesters of pregnancy. Instruct patient to immediately inform her healthcare provider if she is breastfeeding or planning to breastfeed. It is not known if Dapaformin is excreted in breast milk; however, based on animal data, Dapaformin may cause harm to nursing infants. Inform patients that the most common adverse reactions associated with use of Dapaformin are female genital mycotic infections, nasopharyngitis, urinary tract infections, diarrhea, headache, nausea, and vomiting. Instruct patients that Dapaformin must be swallowed whole and not crushed or chewed, and that the inactive ingredients may occasionally be eliminated in the feces as a soft mass that may resemble the original tablet. Instruct patients to take Dapaformin only as prescribed. If a dose is missed, advise patients to take it as soon as it is remembered unless it is almost time for the next dose, in which case patients should skip the missed dose and take the medicine at the next regularly scheduled time. Advise patients not to take 2 tablets of Dapaformin at the same time, unless otherwise instructed by their healthcare provider.
12.0 Date of revision
02 June 2022
About leaflet
Read all of this leaflet carefully before you start taking this medicine because it contains important information for you.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor, pharmacist or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
What is in this leaflet
- What DapaFormin 500/1000 is and what it is used for
- What you need to know before you take DapaFormin 500/1000
- How to take DapaFormin 500/1000 Possible side effects
- How to store DapaFormin 500/1000
- Contents of the pack and other information
1. What DapaFormin 500/1000 is and what it is used for
This medicine contains two different substances called dapagliflozin and metformin. Both belong to a group of medicines called oral anti-diabetics. These are medicines taken by mouth for diabetes.
DapaFormin 500/1000 is used for a type of diabetes called “type 2 diabetes” in adult patients (aged 18 years and older) and usually occurs when you are older. If you have type 2 diabetes, your pancreas does not make enough insulin or your body is not able to use the insulin it produces properly. This leads to a high level of sugar (glucose) in your blood.
- Dapagliflozin works by removing excess sugar from your body via your urine and lowers the amount of sugar in your blood. It can also help prevent heart disease.
- Metformin works mainly by inhibiting glucose production in the liver.
To treat diabetes:
- This medicine is taken in combination with diet and exercise.
- This medicine is used if your diabetes cannot be controlled with other medicines used to treat diabetes.
- Your doctor may ask you to take this medicine on its own or together with other medicines to treat diabetes.
- This may be another medicine taken by mouth and/or a medicine given by injection, such as insulin or a GLP-1 receptor agonist (helps your body to increase the production of insulin when your blood sugar is high).
- If you are already taking both dapagliflozin and metformin as single tablets, your doctor may ask you to switch to this medicine.
- To avoid overdose, do not continue taking dapagliflozin and metformin tablets, if you are taking DapaFormin 500/1000.
It is important to continue to follow the advice on diet and exercise given to you by your doctor, pharmacist or nurse.
2. What you need to know before you take DapaFormin 500/1000
Do not take DapaFormin 500/1000
- if you are allergic to dapagliflozin, metformin or any of the other ingredients of this medicine (listed in section 6).
- if you have ever had a diabetic coma.
- if you have uncontrolled diabetes, with, for example severe hyperglycaemia (high blood glucose), nausea, vomiting, diarrhoea, rapid weight loss, lactic acidosis (see “Risk of lactic acidosis” below) or ketoacidosis. Ketoacidosis is a condition in which substances called ‘ketone bodies’ accumulate in the blood and which can lead to a diabetic pre-coma. Symptoms include stomach pain, fast and deep breathing, sleepiness or your breath developing an unusual fruity smell.
- if you have severely reduced kidney function.
- if you have a severe infection.
- if you have lost a lot of water from your body (dehydration), e.g. due to long-lasting or severe diarrhoea, or if you have vomited several times in a row.
- if you have recently had a heart attack or if you have heart failure or serious problems with your blood circulation or difficulties in breathing.
- if you have problems with your liver.
- if you drink large amounts of alcohol, either every day or only from time to time (please see section “DapaFormin 500/1000 with alcohol”).
Do not take this medicine if any of the above apply to you.
Warnings and precautions
Risk of lactic acidosis
DapaFormin 500/1000 may cause a very rare, but very serious side effect called lactic acidosis, particularly if your kidneys are not working properly. The risk of developing lactic acidosis is also increased with uncontrolled diabetes, serious infections, prolonged fasting or alcohol intake, dehydration (see further information below), liver problems and any medical conditions in which a part of the body has a reduced supply of oxygen (such as acute severe heart disease). If any of the above apply to you, talk to your doctor for further instructions.
Stop taking DapaFormin 500/1000 for a short time if you have a condition that may be associated with dehydration (significant loss of body fluids) such as severe vomiting, diarrhoea, fever, exposure to heat or if you drink less fluid than normal. Talk to your doctor for further instructions.
Stop taking DapaFormin 500/1000 and contact a doctor or the nearest hospital immediately if you experience some of the symptoms of lactic acidosis, as this condition may lead to coma. Symptoms of lactic acidosis include:
- vomiting
- stomach ache (abdominal pain)
- muscle cramps
- a general feeling of not being well with severe tiredness - difficulty in breathing
- reduced body temperature and heartbeat
- Lactic acidosis is a medical emergency and must be treated in a hospital.
Talk to your doctor, pharmacist or nurse before taking DapaFormin 500/1000, and during treatment:
if you have “type 1 diabetes” – the type that usually starts when you are young, and your body does not produce any insulin. DapaFormin 500/1000 should not be used to treat this condition.
if you experience rapid weight loss, feeling sick or being sick, stomach pain, excessive thirst, fast and deep breathing, confusion, unusual sleepiness or tiredness, a sweet smell to your breath, a sweet or metallic taste in your mouth, or a different odour to your urine or sweat, contact a doctor or the nearest hospital straight away. These symptoms could be a sign of “diabetic ketoacidosis” – a rare but serious, sometimes life-threatening problem you can get with diabetes because of increased levels of “ketone bodies” in your urine or blood, seen in tests. The risk of developing diabetic ketoacidosis may be increased with prolonged fasting, excessive alcohol consumption, dehydration, sudden reductions in insulin dose, or a higher need of insulin due to major surgery or serious illness.
if you have problems with your kidneys. Your doctor will check your kidney function.
if you have very high levels of glucose in your blood which may make you dehydrated (lose too much body fluid). Possible signs of dehydration are listed at the top of section 4. Tell your doctor before you start taking this medicine if you have any of these signs.
if you are taking medicines to lower blood pressure (anti-hypertensives) and have a history of low blood pressure (hypotension). More information is given below under ‘Other medicines and DapaFormin 500/1000’.
if you often get infections of the urinary tract. This medicine may cause urinary tract infections and your doctor may want to monitor you more closely. Your doctor may consider temporarily changing your treatment if you develop a serious infection.
If you need to have major surgery, you must stop taking DapaFormin 500/1000 during and for some time after the procedure. Your doctor will decide when you must stop and when to restart your treatment with DapaFormin 500/1000.
It is important to check your feet regularly and adhere to any other advice regarding foot care given by your health care professional.
If any of the above applies to you (or you are not sure), talk to your doctor, pharmacist or nurse before taking this medicine.
Talk to your doctor immediately if you develop a combination of symptoms of pain, tenderness, redness, or swelling of the genitals or the area between the genitals and the anus with fever or feeling generally unwell. These symptoms could be a sign of a rare but serious or even life-threatening infection, called necrotising fasciitis of the perineum or Fournier’s gangrene which destroys the tissue under the skin. Fournier’s gangrene has to be treated immediately.
Kidney function
During treatment with DapaFormin 500/1000, your doctor will check your kidney function at least once every year or more frequently if you are elderly and/or if you have worsening kidney function.
Urine glucose
Because of how this medicine works, your urine will test positive for sugar while you are on this medicine.
Children and adolescents
This medicine is not recommended for children and adolescents under 18 years of age, because it has not been studied in these patients.
Other medicines and DapaFormin 500/1000
If you need to have an injection of a contrast medium that contains iodine into your bloodstream, for example in the context of an X-ray or scan, you must stop taking DapaFormin 500/1000 before or at the time of the injection. Your doctor will decide when you must stop and when to restart your treatment with DapaFormin 500/1000.
Tell your doctor if you are taking, have recently taken or might take any other medicines. You may need more frequent blood glucose and kidney function tests, or your doctor may adjust the dosage of DapaFormin 500/1000. It is especially important to mention the following:
- if you are taking medicines which increase urine production (diuretics).
- Your doctor may ask you to stop taking this medicine. Possible signs of losing too much fluid from your body are listed at the top of section 4.
- if you are taking other medicines that lower the amount of sugar in your blood such as insulin or a “sulphonylurea” medicine.
- Your doctor may want to lower the dose of these other medicines, to prevent you from getting blood sugar levels that are too low (hypoglycaemia). if you are taking cimetidine, a medicine used to treat stomach problems.
- if you are using bronchodilators (beta-2 agonists) which are used to treat asthma.
- if you are using corticosteroids (used to treat inflammation in diseases like asthma and arthritis) that are given by mouth, as an injection, or inhaled.
- if you are using medicines used to treat pain and inflammation (NSAID and COX-2-inhibitors, such as ibuprofen and celecoxib).
- if you are using certain medicines for the treatment of high blood pressure (ACE inhibitors and angiotensin II receptor antagonists).
DapaFormin 500/1000 with alcohol
Avoid excessive alcohol intake while taking DapaFormin 500/1000 since this may increase the risk of lactic acidosis (see “Warnings and precautions”).
Pregnancy and breast-feeding
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine. You should stop taking this medicine if you become pregnant, since it is not recommended during the second and third trimesters (the last six months) of pregnancy. Talk to your doctor about the best way to control your blood sugar while you are pregnant.
Talk to your doctor if you would like to or are breast-feeding before taking this medicine. You should not use this medicine if you are breast-feeding. Metformin passes into human milk in small amounts. It is not known if dapagliflozin passes into human breast milk.
Driving and using machines
This medicine has no or negligible influence on the ability to drive and use machines. Taking it with other medicines that lower the amount of sugar in your blood, such as insulin or a “sulphonylurea” medicine, can cause too low blood sugar levels (hypoglycaemia), which may cause symptoms such as weakness, dizziness, increased sweating, fast heart beat, change in vision or difficulties concentrating, and may affect your ability to drive and use machines. Do not drive or use any tools or machines, if you start to feel these symptoms.
Sodium content
This medicine contains less than 1 mmol sodium (23 mg) per dose, that is to say it is essentially ‘sodiumfree’.
3. How to take DapaFormin 500/1000
Always take this medicine exactly as your doctor has told you. Check with your doctor or pharmacist if you are not sure.
How much to take
- The amount of this medicine that you will take varies depending on your condition and the doses you currently take of metformin and/or individual tablets of dapagliflozin and metformin. Your doctor will tell you exactly which strength of this medicine to take.
- The recommended dose is one tablet twice a day.
Taking this medicine
- Swallow the tablet whole with half a glass of water.
- Take your tablet with food. This is to reduce the risk of side effects in the stomach.
- Take your tablet twice daily, once in the morning (breakfast) and once in the evening (dinner).
Your doctor may prescribe this medicine together with other medicine(s) to lower the amount of sugar in your blood. These may be medicine(s) by mouth or given by injection, such as insulin or a GLP-1 receptor agonist. Remember to take these other medicine(s) as your doctor has told you. This will help get the best results for your health.
Diet and exercise
To control your diabetes, you still need to keep to diet and exercise, even when you are taking this medicine. So it is important to keep following the advice about diet and exercise from your doctor, pharmacist or nurse. In particular, if you are following a diabetic weight control diet, continue to follow it while you are taking this medicine.
If you take more DapaFormin 500/1000 than you should
If you take more DapaFormin 500/1000 tablets than you should, you may experience lactic acidosis. Symptoms of lactic acidosis include feeling or being very sick, vomiting, stomach ache, muscular cramps, severe tiredness or difficulty breathing. If this happens to you, you may need immediate hospital treatment, as lactic acidosis may lead to coma. Stop taking this medicine immediately and contact a doctor or the nearest hospital straight away (see section 2). Take the medicine pack with you.
If you forget to take DapaFormin 500/1000
If you miss a dose, take it as soon as you remember. If you do not remember until it is time for your next dose, skip the missed dose and go back to your regular schedule. Do not take a double dose of this medicine to make up for a forgotten dose.
If you stop taking DapaFormin 500/1000
Do not stop taking this medicine without talking to your doctor first. Your blood sugar may increase without this medicine.
If you have any further questions on the use of this medicine, ask your doctor, pharmacist or nurse.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Stop taking DapaFormin 500/1000 and see a doctor straight away if you notice any of the following serious or potentially serious side effects:
Lactic acidosis, seen very rarely (may affect up to 1 in 10,000 people) DapaFormin 500/1000 may cause a very rare, but very serious side effect called lactic acidosis (see section “Warnings and precautions”). If this happens you must stop taking DapaFormin
500/1000 and contact a doctor or the nearest hospital immediately, as lactic acidosis may lead to coma
Contact a doctor or the nearest hospital straight away if you have any of the following side effects:
Diabetic ketoacidosis, seen rarely (may affect up to 1 in 1,000 people) These are the signs of diabetic ketoacidosis (see also section 2 Warnings and precautions): - increased levels of “ketone bodies” in your urine or blood
rapid weight loss feeling sick or being sick stomach pain excessive thirst fast and deep breathing confusion unusual sleepiness or tiredness a sweet smell to your breath, a sweet or metallic taste in your mouth or a different odour to your urine or sweat.
This may occur regardless of blood glucose level. Your doctor may decide to temporarily or permanently stop your treatment with DapaFormin 500/1000.
Stop taking DapaFormin 500/1000 and see a doctor as soon as possible if you notice any of the following serious or potentially serious effects:
Dehydration: loss of too much fluid from your body, seen uncommonly (may affect up to 1 in 100 people).
These are signs of dehydration:
very dry or sticky mouth, feeling very thirsty feeling very sleepy or tired - passing little or no water (urine) - fast heartbeat.
Urinary tract infection, seen commonly (may affect up to 1 in 10 people). These are signs of a severe infection of the urinary tract: - fever and/or chills
burning sensation when passing water (urinating) - pain in your back or side. Although uncommon, if you see blood in your urine, tell your doctor immediately.
Contact your doctor as soon as possible if you have any of the following side effects:
Low blood sugar levels (hypoglycaemia), seen very commonly (may affect more than 1 in 10 people) - when taking this medicine with a sulphonylurea or other medicines that lower the amount of sugar in your blood, such as insulin.
These are the signs of low blood sugar:
- shaking, sweating, feeling very anxious, fast heart beat - feeling hungry, headache, change in vision
- a change in your mood or feeling confused.
Your doctor will tell you how to treat low blood sugar levels and what to do if you get any of the signs above. If you have symptoms of low blood sugar, eat glucose tablets, a high sugar snack or drink fruit juice. Measure your blood sugar if possible and rest.
Other side effects include:
Very common
- nausea, vomiting
- diarrhoea or stomach ache
- loss of appetite
Common
- genital infection (thrush) of your penis or vagina (signs may include irritation, itching, unusual discharge or odour)
- back pain
- discomfort when passing water (urine), passing more water than usual or needing to pass water more often
- changes in the amount of cholesterol or fats in your blood (shown in tests)
- increases in the amount of red blood cells in your blood (shown in tests)
- decreases in creatinine renal clearance (shown in tests) in the beginning of treatment
- changes in taste dizziness rash
Uncommon
- thirst
- constipation
- awakening from sleep at night to pass urine
- dry mouth
- weight decreased
- increases in creatinine (shown in laboratory blood tests) in the beginning of treatment
- increases in urea (shown in laboratory blood tests)
Very rare
- decreased vitamin B12 levels in the blood
- abnormalities in liver function tests, inflammation of the liver (hepatitis) • redness of the skin (erythema), itching or an itchy rash (hives)
Reporting of side effects
If you get any side effects, talk to your doctor. This includes any possible side effects not listed in this leaflet. You can also report side effects directly: Website: www.zuventus.com and click the tab “Safety Reporting” located on the top right end of the home page.
By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store DapaFormin 500/1000
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date which is stated on the blister or carton after ‘EXP’. The expiry date refers to the last day of that month.
This medicine does not require any special storage conditions.
Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help protect the environment.
6. Contents of the pack and other information
What DapaFormin 500/1000 contains
DapaFormin 500
Each film coated tablet contains :
Monohydrate
equivalent to Dapagliflozin 10 mg
Excipients q.s.
Colours : Titanium Dioxide IP & Ferric Oxide Yellow USP-NF
DapaFormin 1000
Each film coated tablet contains :
Dapagliflozin Propanediol
equivalent to Dapagliflozin 10 mg
Metformin Hydrochloride IP 1000 mg
(Extended Release)
Excipients q.s.