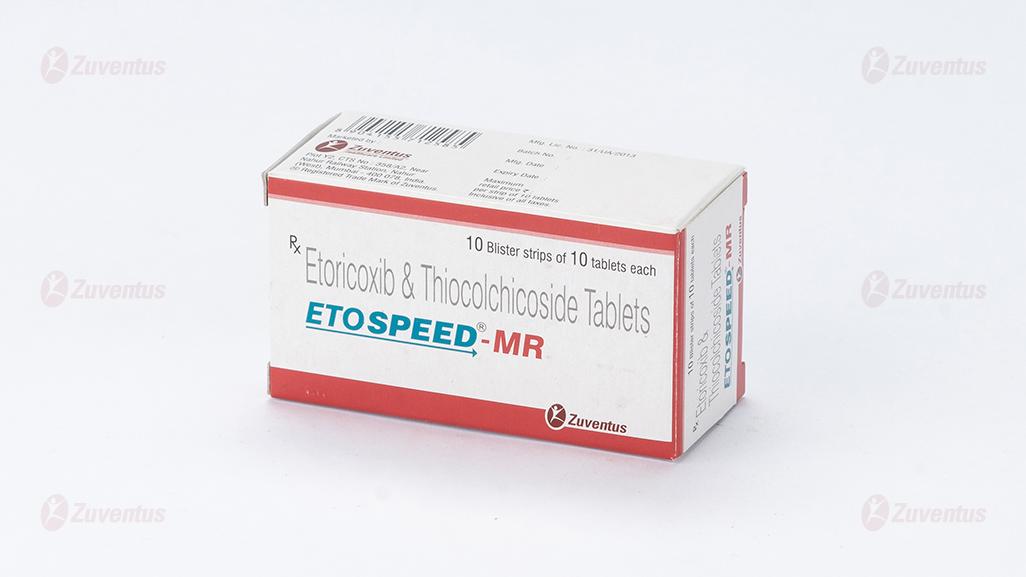
Etospeed MR Tablets
Therapy Area
Pain management
1.0 Generic Name
Etoricoxib & Thiocolchicoside Tablets
2.0 Qualitative and quantitative composition
Composition:
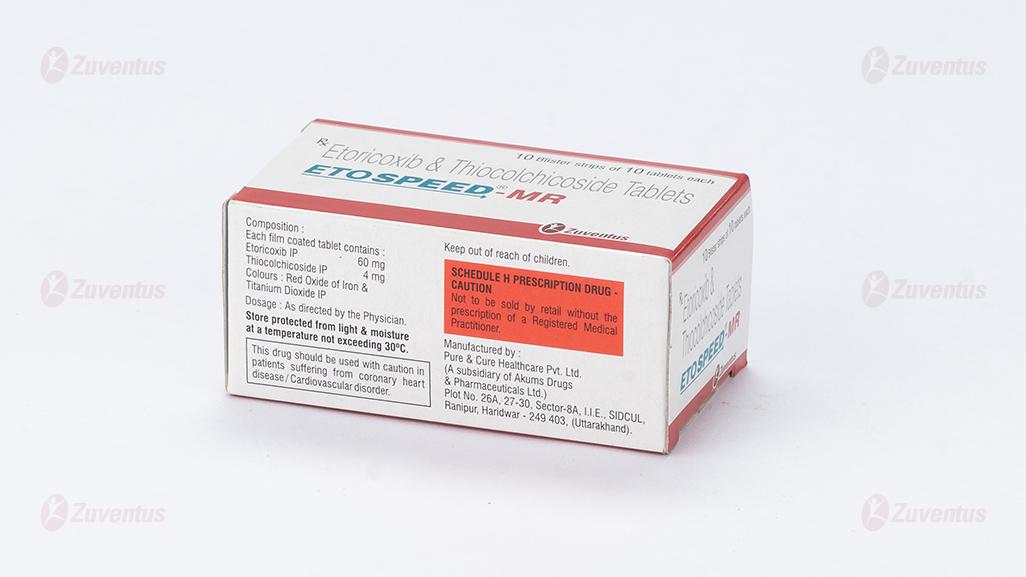
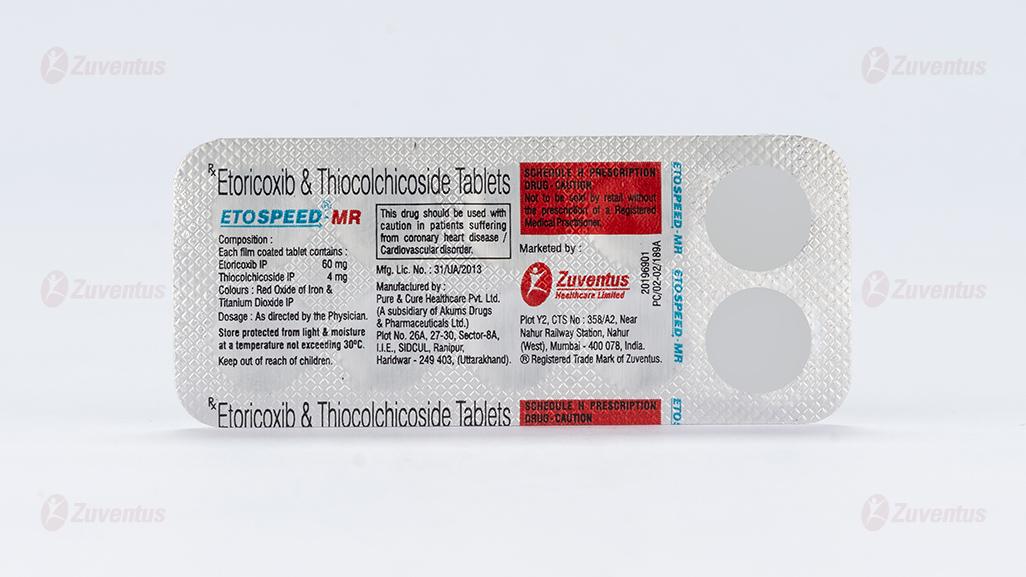
Each film coated tablet contains:
Etoricoxib IP 60 mg
Thiocolchicoside IP 4 mg
Colours: Red Oxide of Iron & Titanium Dioxide IP
3.0 Dosage form and strength
Film coated tablet,
Etoricoxib (60 mg) &Thiocolchicoside (4 mg)
4.0 Clinical particulars
4.1 Therapeutic Indication
For the acute treatment of inflammatory musculoskeletal disorders associated with painful muscle spasm in adults.
4.2 Posology and Method of Administration
One table of ETOSPEED-MR one or two times daily or as prescribed by the healthcare professional depending on the severity of the condition being treated.
4.3 Contraindications
- Hypersensitivity to the active substance or to any of the excipients.
- Active peptic ulceration or active gastro-intestinal (GI) bleeding.
- Patients who, after taking acetylsalicylic acid or NSAIDs including COX-2 inhibitors, experience bronchospasm, acute rhinitis, nasal polyps, angioneurotic oedema, urticaria, or allergic-type reactions.
- Pregnancy and lactation.
- Severe hepatic dysfunction (serum albumin <25 g/l or Child-Pugh score ≥10).
- Estimated renal creatinine clearance < 30 ml/min
- Children and adolescents under 16 years of age.
- Inflammatory bowel disease.
- Congestive heart failure (NYHA II-IV).
- Patients with hypertension whose blood pressure is persistently elevated above 140/90 mmHg and has not been adequately controlled.
- Established ischaemic heart disease, peripheral arterial disease, and cerebrovascular disease.
- In patients with flaccid paralysis, hypotone muscle.
- In women of childbearing potential not using contraception.
4.4 Special warnings and precautions for use
Etoricoxib
Gastrointestinal effects
Upper gastrointestinal complications [perforations, ulcers or bleedings (PUBs)], some of them resulting in fatal outcome, have occurred in patients treated with etoricoxib.
Caution is advised with treatment of patients most at risk of developing a gastrointestinal complication with NSAIDs; the elderly, patients using any other NSAID or acetylsalicylic acid concomitantly or patients with a prior history of gastrointestinal disease, such as ulceration and GI bleeding.
There is a further increase in the risk of gastrointestinal adverse effects (gastrointestinal ulceration or other gastrointestinal complications) when etoricoxib is taken concomitantly with acetylsalicylic acid (even at low doses). A significant difference in GI safety between selective COX-2 inhibitors + acetylsalicylic acid vs. NSAIDs + acetylsalicylic acid has not been demonstrated in long-term clinical trials.
Cardiovascular effects
Clinical trials suggest that the selective COX-2 inhibitor class of drugs may be associated with a risk of thrombotic events (especially myocardial infarction (MI) and stroke), relative to placebo and some NSAIDs. As the cardiovascular risks of etoricoxib may increase with dose and duration of exposure, the shortest duration possible and the lowest effective daily dose should be used. The patient's need for symptomatic relief and response to therapy should be re-evaluated periodically, especially in patients with osteoarthritis.
Patients with significant risk factors for cardiovascular events (e.g. hypertension, hyperlipidaemia, diabetes mellitus, and smoking) should only be treated with etoricoxib after careful consideration.
COX-2 selective inhibitors are not a substitute for acetylsalicylic acid for prophylaxis of cardiovascular Thrombo-embolic diseases because of their lack of antiplatelet effect. Therefore, antiplatelet therapies should not be discontinued
Renal effects
Renal prostaglandins may play a compensatory role in the maintenance of renal perfusion. Therefore, under conditions of compromised renal perfusion, administration of etoricoxib may cause a reduction in prostaglandin formation and, secondarily, in renal blood flow, and thereby impair renal function. Patients at greatest risk of this response are those with pre-existing significantly impaired renal function, uncompensated heart failure, or cirrhosis. Monitoring of renal function in such patients should be considered.
Fluid retention, oedema and hypertension
As with other medicinal products known to inhibit prostaglandin synthesis, fluid retention, oedema and hypertension have been observed in patients taking etoricoxib. All Nonsteroidal Anti-inflammatory Drugs (NSAIDs), including etoricoxib, can be associated with new onset or recurrent congestive heart failure. For information regarding a dose related response for etoricoxib. Caution should be exercised in patients with a history of cardiac failure, left ventricular dysfunction, or hypertension and in patients with pre-existing oedema from any other reason. If there is clinical evidence of deterioration in the condition of these patients, appropriate measures including discontinuation of etoricoxib should be taken.
Etoricoxib may be associated with more frequent and severe hypertension than some other NSAIDs and selective COX-2 inhibitors, particularly at high doses. Therefore, hypertension should be controlled before treatment with etoricoxib and special attention should be paid to blood pressure monitoring during treatment with etoricoxib. Blood pressure should be monitored within two weeks after initiation of treatment and periodically thereafter. If blood pressure rises significantly, alternative treatment should be considered.
Hepatic effects
Elevations of alanine aminotransferase (ALT) and/or aspartate aminotransferase (AST) (approximately three or more times the upper limit of normal) have been reported in approximately 1% of patients in clinical trials treated for up to one year with etoricoxib 30, 60 and 90 mg daily.
Any patients with symptoms and/or signs suggesting liver dysfunction, or in whom an abnormal liver function test has occurred, should be monitored. If signs of hepatic insufficiency occur, or if persistently abnormal liver function tests (three times the upper limit of normal) are detected, etoricoxib should be discontinued.
General
If during treatment, patients deteriorate in any of the organ system functions described above, appropriate measures should be taken and discontinuation of etoricoxib therapy should be considered. Medically appropriate supervision should be maintained when using etoricoxib in the elderly and in patients with renal, hepatic, or cardiac dysfunction.
Caution should be used when initiating treatment with etoricoxib in patients with dehydration. It is advisable to rehydrate patients prior to starting therapy with etoricoxib. Serious skin reactions, some of them fatal, including exfoliative dermatitis, Stevens Johnson syndrome, and toxic epidermal necrolysis, have been reported very rarely in association with the use of NSAIDs and some selective COX-2 inhibitors during post-marketing surveillance. Patients appear to be at highest risk for these reactions early in the course of therapy with the onset of the reaction occurring in the majority of cases within the first month of treatment. Serious hypersensitivity reactions (such as anaphylaxis and angioedema) have been reported in patients receiving etoricoxib. Some selective COX-2 inhibitors have been associated with an increased risk of skin reactions in patients with a history of any drug allergy. Etoricoxib should be discontinued at the first appearance of skin rash, mucosal lesions, or any other sign of hypersensitivity.
Etoricoxib may mask fever and other signs of inflammation.
Caution should be exercised when co-administering etoricoxib with warfarin or other oral anticoagulants.
The use of etoricoxib, as with any medicinal product known to inhibit cyclooxygenase / prostaglandin synthesis, is not recommended in women attempting to conceive.
ETOSPEED-MR Tablets contain lactose. Patients with rare hereditary problems of galactose intolerance, the Lapp lactase deficiency or glucose-galactose malabsorption should not take this medicine.
Thiocolchicoside
The dose must be reduced in case of presence of diarrhoea following oral administration. After administration by intramuscular route episodes were observed of vasovagal syncope, thus the patient has to be monitored after being injected.
Post marketing cases of cytolytic hepatitis and cholestatic were reported with Thiocolchicoside.
The serious cases (for example fulminant hepatitis) were observed in patients that had taken FANS or paracetamol at the same time. The patients have to be informed to report any sign of hepatic toxicity.
Thiocolchicoside may precipitate seizures especially in epileptic patients or those at risk of convulsions.
The maximum daily oral dose of 16mg must not be exceeded and must be split in two doses at 12-hour interval.
In case you forget to take a dose take the next dose avoiding taking doses close to each other.
Preclinical studies showed that one of Thiocolchicoside metabolites (SL59.0955) induced aneuploidy (i.e. alterations in the number of chromosomes in dividing cells) at concentrations close to human exposure observed at doses 8 mg twice daily per os. Aneuploidy is considered as a risk factor for teratogenicity, embryo/foetotoxicity, spontaneous abortion, and impaired male fertility and a potential risk factor for cancer. As a precautionary measure, use of the product at doses exceeding the recommended dose or long-term use should be avoided.
Patients should be carefully informed about the potential risk of a possible pregnancy and about effective contraception measures to be followed.
4.5 Drugs interactions
Etoricoxib
Pharmacodynamic interactions
Oral anticoagulants: In subjects stabilised on chronic warfarin therapy, the administration of etoricoxib 120 mg daily was associated with an approximate 13% increase in prothrombin time International Normalised Ratio (INR). Therefore, patients receiving oral anticoagulants should be closely monitored for their prothrombin time INR, particularly in the first few days when therapy with etoricoxib is initiated or the dose of etoricoxib is changed.
Diuretics, ACE inhibitors and Angiotensin II Antagonists: NSAIDs may reduce the effect of diuretics and other antihypertensive drugs. In some patients with compromised renal function (e.g. dehydrated patients or elderly patients with compromised renal function) the co-administration of an ACE inhibitor or Angiotensin II antagonist and agents that inhibit cyclo-oxygenase may result in further deterioration of renal function, including possible acute renal failure, which is usually reversible. These interactions should be considered in patients taking etoricoxib concomitantly with ACE inhibitors or angiotensin II antagonists. Therefore, the combination should be administered with caution, especially in the elderly. Patients should be adequately hydrated and consideration should be given to monitoring of renal function after initiation of concomitant therapy, and periodically thereafter.
Acetylsalicylic Acid: In a study in healthy subjects, at steady state, etoricoxib 120 mg once daily had no effect on the anti-platelet activity of acetylsalicylic acid (81 mg once daily). Etoricoxib can be used concomitantly with acetylsalicylic acid at doses used for cardiovascular prophylaxis (low-dose acetylsalicylic acid). However, concomitant administration of low-dose acetylsalicylic acid with etoricoxib may result in an increased rate of GI ulceration or other complications compared to use of etoricoxib alone. Concomitant administration of etoricoxib with doses of acetylsalicylic acid above those for cardiovascular prophylaxis or with other NSAIDs is not recommended.
Cyclosporin and tacrolimus: Although this interaction has not been studied with etoricoxib, coadministration of cyclosporin or tacrolimus with any NSAID may increase the nephrotoxic effect of cyclosporin or tacrolimus. Renal function should be monitored when etoricoxib and either of these drugs is used in combination.
Pharmacokinetic interactions
The effect of etoricoxib on the pharmacokinetics of other drugs.
Lithium: NSAIDs decrease lithium renal excretion and therefore increase lithium plasma levels. If necessary, monitor blood lithium closely and adjust the lithium dosage while the combination is being taken and when the NSAID is withdrawn.
Methotrexate: Two studies investigated the effects of etoricoxib 60, 90 or 120 mg administered once daily for seven days in patients receiving once-weekly methotrexate doses of 7.5 to 20 mg for rheumatoid arthritis. Etoricoxib at 60 and 90 mg had no effect on methotrexate plasma concentrations or renal clearance. In one study, etoricoxib 120 mg had no effect, but in the other study, etoricoxib 120 mg increased methotrexate plasma concentrations by 28% and reduced renal clearance of methotrexate by 13%.
Adequate monitoring for methotrexate-related toxicity is recommended when etoricoxib and methotrexate are administered concomitantly.
Oral contraceptives: Etoricoxib 60 mg given concomitantly with an oral contraceptive containing 35 micrograms ethinyl estradiol (EE) and 0.5 to 1 mg norethindrone for 21 days increased the steady state AUC0-24hr of EE by 37%. Etoricoxib 120 mg given with the same oral contraceptive concomitantly or separated by 12 hours, increased the steady state AUC0-24hr of EE by 50 to 60%. This increase in EE concentration should be considered when selecting an oral contraceptive for use with etoricoxib. An increase in EE exposure can increase the incidence of adverse events associated with oral contraceptives (e.g., venous Thrombo-embolic events in women at risk).
Hormone Replacement Therapy (HRT): Administration of etoricoxib 120 mg with hormone replacement therapy consisting of conjugated estrogens (0.625 mg) for 28 days, increased the mean steady state AUC0-24hr of unconjugated estrone (41%), equilin (76%), and 17-β-estradiol (22%). The effect of the recommended chronic doses of etoricoxib (30, 60, and 90 mg) has not been studied. The effects of etoricoxib 120 mg on the exposure (AUC0-24hr) to these estrogenic components of PREMARIN were less than half of those observed when PREMARIN was administered alone and the dose was increased from 0.625 to 1.25 mg. The clinical significance of these increases is unknown, and higher doses of PREMARIN were not studied in combination with etoricoxib. These increases in estrogenic concentration should be taken into consideration when selecting post-menopausal hormone therapy for use with etoricoxib because the increase in oestrogen exposure might increase the risk of adverse events associated with HRT.
Prednisone/prednisolone: In drug-interaction studies, etoricoxib did not have clinically important effects on the pharmacokinetics of prednisone/prednisolone.
Digoxin: Etoricoxib 120 mg administered once daily for 10 days to healthy volunteers did not alter the steady-state plasma AUC0-24hr or renal elimination of digoxin. There was an increase in digoxin Cmax (approximately 33%). This increase is not generally important for most patients. However, patients at high risk of digoxin toxicity should be monitored for this when etoricoxib and digoxin are administered concomitantly.
Effect of etoricoxib on drugs metabolised by sulfotransferases
Etoricoxib is an inhibitor of human sulfotransferase activity, particularly SULT1E1, and has been shown to increase the serum concentrations of ethinyl estradiol. While knowledge about effects of multiple sulfotransferases is presently limited and the clinical consequences for many drugs are still being examined, it may be prudent to exercise care when administering etoricoxib concurrently with other drugs primarily metabolised by human sulfotransferases (e.g., oral salbutamol and minoxidil).
Effect of etoricoxib on drugs metabolised by CYP isoenzymes
Based on in vitro studies, etoricoxib is not expected to inhibit cytochromes P450 (CYP) 1A2, 2C9, 2C19, 2D6, 2E1 or 3A4. In a study in healthy subjects, daily administration of etoricoxib 120 mg did not alter hepatic CYP3A4 activity as assessed by the erythromycin breath test.
Effects of other drugs on the pharmacokinetics of etoricoxib
The main pathway of etoricoxib metabolism is dependent on CYP enzymes. CYP3A4 appears to contribute to the metabolism of etoricoxib in vivo. In vitro studies indicate that CYP2D6, CYP2C9, CYP1A2 and CYP2C19 also can catalyse the main metabolic pathway, but their quantitative roles have not been studied in vivo.
Ketoconazole: Ketoconazole, a potent inhibitor of CYP3A4, dosed at 400 mg once a day for 11 days to healthy volunteers, did not have any clinically important effect on the single-dose pharmacokinetics of 60 mg etoricoxib (43% increase in AUC).
Voriconazole and Miconazole: Co-administration of either oral voriconazole or topical miconazole oral gel, strong CYP3A4 inhibitors, with etoricoxib caused a slight increase in exposure to etoricoxib, but is not considered to be clinically meaningful based on published data.
Rifampicin: Co-administration of etoricoxib with rifampicin, a potent inducer of CYP enzymes, produced a 65% decrease in etoricoxib plasma concentrations. This interaction may result in recurrence of symptoms when etoricoxib is co-administered with rifampicin. While this information may suggest an increase in dose, doses of etoricoxib greater than those listed for each indication have not been studied in combination with rifampicin and are therefore not recommended.
Antacids: Antacids do not affect the pharmacokinetics of etoricoxib to a clinically relevant extent.
Thiocolchicoside
No studies on interactions were carried out.
4.6 Use in special populations
Pregnancy
Etoricoxib
No clinical data on exposed pregnancies are available for etoricoxib. Studies in animals have shown reproductive toxicity. The potential for human risk in pregnancy is unknown. Etoricoxib, as with other medicinal products inhibiting prostaglandin synthesis, may cause uterine inertia and premature closure of the ductus arteriosus during the last trimester. Etoricoxib is contraindicated in pregnancy. If a woman becomes pregnant during treatment, etoricoxib must be discontinued.
Thiocolchicoside
There are limited data on the use of Thiocolchicoside in pregnant women. Therefore, the potential hazards for the embryo and foetus are unknown. Studies in animals have shown teratogenic effects.
Therefore, ETOSPEED-MR is contraindicated during pregnancy and in women of childbearing potential not using contraception
Lactation:
Etoricoxib
It is not known whether etoricoxib is excreted in human milk. Etoricoxib is excreted in the milk of lactating rats. Women who use etoricoxib must not breast feed.
Thiocolchicoside
Since it passes into the mother’s milk, the use of Thiocolchicoside is contraindicated during breastfeeding.
Therefore, ETOSPEED-MR is contraindicated during breastfeeding.
Fertility
The use of etoricoxib, as with any drug substance known to inhibit COX-2, is not recommended in women attempting to conceive.
In a fertility study performed in rats, no impairment of fertility was seen at doses up to 12 mg/kg, i.e. at dose levels inducing no clinical effect. Thiocolchicoside and its metabolites exert aneugenic activity at different concentration levels, which is a risk factor for impairment of human fertility.
Therefore, ETOSPEED-MR is contraindicated in women attempting to conceive.
4.7 Effects on ability to drive and use machines
Patients who experience dizziness, vertigo or somnolence while taking etoricoxib should refrain from driving or operating machinery. No studies were carried out on the ability to drive or use of machinery with Thiocolchicoside.
So if drowsiness occurs with ETOSPEED-MR, patients must refrain from driving or operating machinery.
4.8 Undesirable effects
Etoricoxib
Summary of the safety profile
In clinical trials, etoricoxib was evaluated for safety in 9,295 individuals, including 6,757 patients with OA, RA, chronic low back pain or ankylosing spondylitis (approx..600 patients with OA or RA were treated for one year or longer).
In clinical studies, the undesirable effects profile was similar in patients with OA or RA treated with etoricoxib for one year or longer.
In a clinical study for acute gouty arthritis, patients were treated with etoricoxib 120 mg once daily for eight days. The adverse experience profile in this study was generally similar to that reported in the combined OA, RA, and chronic low back pain studies.
In a cardiovascular safety outcomes programme of pooled data from three active comparator controlled trials, 17, 412 patients with OA or RA were treated with etoricoxib (60 mg or 90 mg) for a mean duration of approximately 18 months. The safety data and details from this programme.
In clinical studies for acute postoperative dental pain following surgery including 614 patients treated with etoricoxib (90 mg or 120 mg), the adverse experience profile in these studies was generally similar to that reported in the combined OA, RA, and chronic low back pain studies.
Tabulated list of adverse reactions
The following undesirable effects were reported at an incidence greater than placebo in clinical trials in patients with OA, RA, chronic low back pain or ankylosing spondylitis treated with etoricoxib 30 mg, 60 mg or 90 mg up to the recommended dose for up to 12 weeks; in the MEDAL Programme studies for up to 3½ years; in short term acute pain studies for up to 7 days; or in post-marketing experience:
The following serious undesirable effects have been reported in association with the use of NSAIDs and cannot be ruled out for etoricoxib: nephrotoxicity including interstitial nephritis and nephrotic syndrome.
Thiocolchicoside
Disturbances in immunity system
Anaphylactic reactions:
- Uncommon: pruritis,
- Rare: urticarial
- Very rare: hypotension
- Not noted: angiooedema and anaphylactic shock after intramuscular administration.
Pathology of the nervous system
- Common: drowsiness
- Rare: agitation and clouding
- Not noted: malaise associated or to a lesser extent vasovagal syncope in the minutes following intramuscular administration, convulsions.
Gastrointestinal pathology
- Common: diarrhoea (see paragraph 4.4), stomach pain
- Uncommon: nausea, vomiting
- Rare: heartburn after oral administration
Hepatobiliary pathology
- Not noted: cytolytic hepatitis and cholestatic.
- Pathology of the skin and subcutaneous tissue
- Uncommon: allergic skin reactions
Reporting of suspected adverse reactions
- Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via email to: medico@zuventus.com
- Website link: https://www.zuventus.com/drug-safety-reporting
4.9 Overdose
Etoricoxib
In clinical studies, administration of single doses of etoricoxib up to 500 mg and multiple doses up to 150 mg/day for 21 days did not result in significant toxicity. There have been reports of acute overdosage with etoricoxib, although adverse experiences were not reported in the majority of cases. The most frequently observed adverse experiences were consistent with the safety profile for etoricoxib (e.g. gastrointestinal events, cardio renal events). In the event of overdose, it is reasonable to employ the usual supportive measures, e.g., remove unabsorbed material from the GI tract, employ clinical monitoring, and institute supportive therapy, if required. Etoricoxib is not dialysable by haemodialysis; it is not known whether etoricoxib is dialysable by peritoneal dialysis.
Thiocolchicoside
Overdosage was not noted or reported in any literature. In case of overdosage it is recommended to get medical attention and implement symptomatic measures.
5.0 Pharmacological properties
5.1 Mechanism of Action
Etoricoxib
Etoricoxib is an oral, selective cyclo-oxygenase-2 (COX-2) inhibitor within the clinical dose range. Across clinical pharmacology studies, ETOSPEED-MR produced dose dependent inhibition of COX-2 without inhibition of COX-1 at doses up to 150 mg daily. Etoricoxib did not inhibit gastric prostaglandin synthesis and had no effect on platelet function. Cyclooxygenase is responsible for generation of prostaglandins. Two isoforms, COX-1 and COX-2, have been identified. COX-2 is the isoform of the enzyme that has been shown to be induced by pro-inflammatory stimuli and has been postulated to be primarily responsible for the synthesis of prostanoid mediators of pain, inflammation, and fever. COX-2 is also involved in ovulation, implantation and closure of the ductus arteriosus, regulation of renal function, and central nervous system functions (fever induction, pain perception and cognitive function). It may also play a role in ulcer healing. COX-2 has been identified in tissue around gastric ulcers in man but its relevance to ulcer healing has not been established.
Thiocolchicoside
Thiocolchicoside binds to GABA-A and strychnine sensitive glycine receptors. Thiocolchicoside acting as a GABA-A receptor antagonist, its myorelaxant effects could be exerted at the supra-spinal level, via complex regulatory mechanisms, although a glycinergic mechanism of action cannot be excluded. The characteristics of the interaction of Thiocolchicoside with GABA-A receptors are qualitatively and quantitatively shared by its main circulating metabolite, the glucuronidated derivative.
5.2 Pharmacodynamic properties
Etoricoxib
In patients with osteoarthritis (OA), etoricoxib 60 mg once daily provided significant improvements in pain and patient assessments of disease status. These beneficial effects were observed as early as the second day of therapy and maintained for up to 52 weeks. Studies with etoricoxib 30 mg once daily demonstrated efficacy superior to placebo over a 12-week treatment period (using similar assessments as the above studies). In a dose ranging study, etoricoxib 60 mg demonstrated significantly greater improvement than 30 mg for all 3 primary endpoints over 6 weeks of treatment. The 30 mg dose has not been studied in osteoarthritis of hands.
In patients with rheumatoid arthritis (RA), etoricoxib 60 mg and 90 mg once daily both provided significant improvements in pain, inflammation, and mobility. In studies evaluating the 60 mg and 90 mg dose, these beneficial effects were maintained over the 12-week treatment periods. In a study evaluating the 60 mg dose compared to the 90 mg dose, etoricoxib 60 mg once daily and 90 mg once daily were both more effective than placebo. The 90 mg dose was superior to the 60 mg dose for Patient Global Assessment of Pain (0-100 mm visual analogue scale), with an average improvement of -2.71 mm (95 % CI: -4.98 mm, -0.45 mm).
In patients experiencing attacks of acute gouty arthritis, etoricoxib 120 mg once daily over an eight-day treatment period, relieved moderate to extreme joint pain and inflammation comparable to indomethacin 50 mg three times daily. Pain relief was observed as early as four hours after initiation of treatment.
In patients with ankylosing spondylitis, etoricoxib 90 mg once daily provided significant improvements in spine pain, inflammation, stiffness and function. The clinical benefit of etoricoxib was observed as early as the second day of therapy after initiation of treatment and was maintained throughout the 52-week treatment period. In a second study evaluating the 60 mg dose compared to the 90 mg dose, etoricoxib 60 mg daily and 90 mg daily demonstrated similar efficacy compared to naproxen 1,000 mg daily. Among inadequate responders to 60 mg daily for 6 weeks, dose escalation to 90 mg daily improved spinal pain intensity score (0-100 mm visual analogue scale) compared to continuing on 60 mg daily, with an average improvement of -2.70 mm (95 % CI: -4.88 mm, -0.52 mm).
In a clinical study evaluating postoperative dental pain, etoricoxib 90 mg was administered once daily for up to three days. In the subgroup of patients with moderate pain at baseline, etoricoxib 90 mg demonstrated a similar analgesic effect to that of ibuprofen 600 mg (16.11 vs. 16.39; P = 0.722), and greater than that of paracetamol/codeine 600 mg/60 mg (11.00; P < 0.001) and placebo (6.84; P < 0.001) as measured by total pain relief over the first 6 hours (TOPAR6). The proportion of patients reporting rescue medication usage within the first 24 hours of dosing was 40.8 % for etoricoxib 90 mg, 25.5 % for ibuprofen 600 mg Q6h, and 46.7 % for paracetamol/codeine 600 mg/60 mg Q6h compared to 76.2 % for placebo. In this study, the median onset of action (perceptible pain relief) of 90 mg etoricoxib was 28 minutes after dosing.
Thiocolchicoside
Pharmacotherapeutic category: Other muscle relaxant with central action, ATC code: M03BX05
Thiocolchicoside is a semisynthetic sulphide derivative of colchicoside, showing muscle relaxant pharmacological activity.
In vitro thiocolchicoside binds solely with GABA receptors and glycinergic stricnine sensitive. From the moment that thiocolchicoside acts as an antagonist of the GABA receptors, its muscle relaxant effect may be exercised to a supraspinal level, through a regulatory mechanism even though the glycinergic mechanism of action cannot be excluded. The characteristics of interaction with the GABA receptors are qualitative and quantitative divided between thiocolchicoside and its main circulating metabolite, the derivative glucuronidated
In vivo the muscle relaxant properties of thiocolchicoside and its main metabolite have been shown in various predictive models of rat and rabbit.
The lack of muscle relaxant effect of thiocolchicoside in spineless rat suggests apredominant supraspinal activity.
Also electrocephalographic studies have shown that thiocolchicoside and its main metabolite are devoid of any sedative effect.
5.3 Pharmacokinetic properties
Etoricoxib
Absorption
Orally administered etoricoxib is well absorbed. The absolute bioavailability is approximately 100%. Following 120 mg once-daily dosing to steady state, the peak plasma concentration (geometric mean Cmax = 3.6 µg/ml) was observed at approximately 1 hour (Tmax) after administration to fasted adults. The geometric mean area under the curve (AUC0-24hr) was 37.8 µg•hr/ml. The pharmacokinetics of etoricoxib are linear across the clinical dose range.
Dosing with food (a high-fat meal) had no effect on the extent of absorption of etoricoxib after administration of a 120-mg dose. The rate of absorption was affected, resulting in a 36% decrease in Cmax and an increase in Tmax by 2 hours. These data are not considered clinically significant. In clinical trials, etoricoxib was administered without regard to food intake.
Distribution
Etoricoxib is approximately 92% bound to human plasma protein over the range of concentrations of 0.05 to 5 µg/ml. The volume of distribution at steady state (Vdss) was approximately 1,20l in humans.
Etoricoxib crosses the placenta in rats and rabbits, and the blood-brain barrier in rats.
Biotransformation
Etoricoxib is extensively metabolised with < 1% of a dose recovered in urine as the parent drug. The major route of metabolism to form the 6'-hydroxymethyl derivative is catalyzed by CYP enzymes. CYP3A4 appears to contribute to the metabolism of etoricoxib in vivo. In vitro studies indicate that CYP2D6, CYP2C9, CYP1A2 and CYP2C19 also can catalyse the main metabolic pathway, but their quantitative roles in vivo have not been studied. Five metabolites have been identified in man. The principal metabolite is the 6'-carboxylic acid derivative of etoricoxib formed by further oxidation of the 6'- hydroxymethyl derivative. These principal metabolites either demonstrate no measurable activity or are only weakly active as COX-2 inhibitors. None of these metabolites inhibit COX-1.
Elimination
Following administration of a single 25-mg radiolabelled intravenous dose of etoricoxib to healthy subjects, 70% of radioactivity was recovered in urine and 20% in faeces, mostly as metabolites. Less than 2% was recovered as unchanged drug.
Elimination of etoricoxib occurs almost exclusively through metabolism followed by renal excretion. Steady state concentrations of etoricoxib are reached within seven days of once daily administration of 120 mg, with an accumulation ratio of approximately 2, corresponding to a half-life of approximately 22 hours. The plasma clearance after a 25- mg intravenous dose is estimated to be approximately 50 ml/min.
Characteristics in patients
Elderly patients: Pharmacokinetics in the elderly (65 years of age and older) are similar to those in the young.
Gender: The pharmacokinetics of etoricoxib are similar between men and women.
Hepatic impairment: Patients with mild hepatic dysfunction (Child-Pugh score 5-6) administered etoricoxib 60 mg once daily had an approximately 16% higher mean AUC as compared to healthy subjects given the same regimen. Patients with moderate hepatic dysfunction (Child-Pugh score 7-9) administered etoricoxib 60 mg every other day had similar mean AUC to the healthy subjects given etoricoxib 60 mg once daily; etoricoxib 30 mg once daily has not been studied in this population. There are no clinical or pharmacokinetic data in patients with severe hepatic dysfunction (Child-Pugh score ≥10).
Renal impairment: The pharmacokinetics of a single dose of etoricoxib 120 mg in patients with moderate to severe renal insufficiency and patients with end-stage renal disease on haemodialysis were not significantly different from those in healthy subjects. Haemodialysis contributed negligibly to elimination (dialysis clearance approximately 50 ml/min).
Paediatric patients: The pharmacokinetics of etoricoxib in paediatric patients (60 kg given etoricoxib 90 mg once daily were similar to the pharmacokinetics in adults given etoricoxib 90 mg once daily. Safety and effectiveness of etoricoxib in paediatric patients have not been established.
Thiocolchicoside
Absorption
After oral administration, no thiocolchicoside is detected in plasma. Only two metabolites are observed: The pharmacologically active metabolite SL18.0740 and an inactive metabolite SL59.0955.
For both metabolites, maximum plasma concentrations occur 1hour after thiocolchicoside administration. After a single oral dose of 8 mg of thiocolchicoside the Cmax and AUC of SL18.0740 are about 60 ng/mL and 130 ng.h/mL respectively. For SL59.0955 these values are much lower: Cmax around 13 ng/mL and AUC ranging from 15.5 ng.h/mL (until 3h) to 39.7 ng.h/mL (until 24h).
Distribution
The apparent volume of distribution of thiocolchicoside is estimated around 42.7 L after an IM administration of 8 mg. No data are available for both metabolites.
Biotransformation
After oral administration, thiocolchicoside is first metabolized in the aglycon 3- demethyltiocolchicine or SL59.0955. This step mainly occurs by intestinal metabolism explaining the lack of circulating unchanged thiocolchicoside by this route of administration. SL59.0955 is then glucuroconjugated into SL18.0740 which has equipotent pharmacological activity to thiocolchicoside and thus supports the pharmacological activity after oral administration of thiocolchicoside. SL59.0955 is also demethylated into didemethyl-thiocolchicine.
Elimination
After oral administration of thiocolchicoside, the SL18.0740 metabolites is eliminated with an apparent t1/2 ranging from 3.2 to 7 hours and the metabolite SL59.0955 has a t 1/2 averaging 0.8h.
6.0 Nonclinical properties
6.1 Animal Toxicology or Pharmacology
Etoricoxib
In reported preclinical studies, etoricoxib has been demonstrated not to be genotoxic. Etoricoxib was not carcinogenic in mice. Rats developed hepatocellular and thyroid follicular cell adenomas at >2-times the daily human dose [90 mg] based on systemic exposure when dosed daily for approximately two years. Hepatocellular and thyroid follicular cell adenomas observed in rats are considered to be a consequence of rat specific mechanism related to hepatic CYP enzyme induction. Etoricoxib has not been shown to cause hepatic CYP3A enzyme induction in humans.
In the rat, gastrointestinal toxicity of etoricoxib increased with dose and exposure time. In the 14-week toxicity study etoricoxib caused gastrointestinal ulcers at exposures greater than those seen in man at the therapeutic dose. In the 53- and 106-week toxicity study, gastrointestinal ulcers were also seen at exposures comparable to those seen in man at the therapeutic dose. In dogs, renal and gastrointestinal abnormalities were seen at high exposures.
Etoricoxib was not teratogenic in reproductive toxicity studies conducted in rats at 15 mg/kg/day (this represents approximately 1.5 times the daily human dose [90 mg] based on systemic exposure). In rabbits, a treatment related increase in cardiovascular malformations was observed at exposure levels below the clinical exposure at the daily human dose (90 mg). However, no treatment-related external or skeletal foetal malformations were observed. In rats and rabbits, there was a dose dependent increase in post implantation loss at exposures greater than or equal to 1.5 times the human exposure.
Etoricoxib is excreted in the milk of lactating rats at concentrations approximately twofold those in plasma. There was a decrease in pup body weight following exposure of pups to milk from dams administered etoricoxib during lactation.
Thiocolchicoside
Thiocolchicoside profile has been assessed in vitro, and in vivo following parenteral and oral administration. Thiocolchicoside was well tolerated following oral administration for periods of up to 6 months in both the rat and the non-human primate when administered at repeated doses of less than or equal to 2 mg/kg/day in the rat and less or equal to 2.5 mg/kg/day in non-human primate, and by the intramuscular route in the primate at repeated doses up to 0.5 mg/kg/day for 4 weeks. At high doses, thiocolchicoside induced emesis in dog, diarrhoea in rat and convulsions in both rodents and no rodents after acute administration by oral route. After repeated administration, thiocolchicoside induced gastro-intestinal disorders (enteritis, emesis) by oral route and emesis by IM route. Thiocolchicoside itself did not induce gene mutation in bacteria (Ames test), in vitro chromosomal damage (chromosome aberration test in human lymphocytes) and in vivo chromosomal damage (in vivo micronucleus in mouse bone marrow administered intraperitoneally). The major glucuro-conjugated metabolite SL18.0740 did not induce gene mutation in bacteria (Ames test); however, it induced in vitro chromosomal damage (in vitro micronucleus test on human lymphocytes) and in vivo chromosomal damage (in vivo micronucleus test in mouse bone marrow administered orally). The micronuclei predominantly resulted from chromosome loss (centromere positive micronuclei after FISH centromere staining), suggesting aneugenic properties. The aneugenic effect of SL18.0740 was observed at concentrations in the in vitro test and at AUC plasma exposures in the in vivo test higher (more than 10 fold based on AUC) than those observed in human plasma at therapeutic doses. The aglycon metabolite (3-demethylthiocolchicine-SL59.0955) formed mainly after oral administration induced in vitro chromosomal damage (in vitro micronucleus test on human lymphocytes) and in vivo chromosomal damage (in vivo oral micronucleus test in rat bone marrow administered orally). The micronuclei predominantly resulted from chromosome loss (centromere positive micronuclei after FISH or CREST centromere staining), suggesting aneugenic properties. The aneugenic effect of SL59.0955 was observed at concentrations in the in vitro test and at exposures in the in vivo test close to those observed in human plasma at therapeutic doses of 8 mg twice daily per os. Aneugenic effect in dividing cells may result in aneuploid cells. Aneuploidy is a modification in the number of chromosomes and loss of heterozygosity, which is recognized as a risk factor for teratogenicity, embryotoxicity/ spontaneous abortion, impaired male fertility, when impacting germ cells and a potential risk factor for cancer when impacting somatic cells. The presence of the aglycon metabolite (3-23 demethylthiocolchicine-SL59.0955) after intramuscular administration has never been assessed, therefore its formation using this route of administration cannot be excluded. In the rat, an oral dose of 12 mg/kg/day of thiocolchicoside caused major malformations along with fetotoxicity (retarded growth, embryo death, impairment of sex distribution rate). The dose without toxic effect was 3 mg/kg/day. In the rabbit, thiocolchicoside showed maternotoxicity starting from 24 mg/kg/day. Furthermore, minor abnormalities have been observed (supernumerary ribs, retarded ossification). In a fertility study performed in rats, no impairment of fertility was seen at doses up to 12 mg/kg/day, i.e. at dose levels inducing no clinical effect. Thiocolchicoside and its metabolites exert aneugenic activity at different concentration levels, which is recognised as a risk factor for impairment of human fertility. The carcinogenic potential was not evaluated.
7.0 Description
Etoricoxib
Etoricoxib is 5-chloro-2-(6-methyl-3-pyridinyl)-3-(4-methylsufonylphenyl) pyridine having molecular weight of 358.5 and molecular formula is C18H15ClN2O2S and chemical structure is:

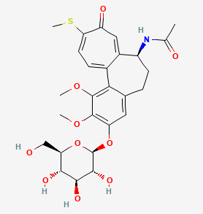
Thiocolchicoside
Thiocolchicoside is chemically N-[(7S)-1,2-dimethoxy-10-methylsulfanyl-9-oxo-3- [(2S,3R,4S,5S,6R)-3,4,5-trihydroxy-6-(hydroxymethyl)oxan-2-yl]oxy-6,7-dihydro-5H- Page 25 of 33 benzo[a]heptalen-7-yl]acetamide having molecular weight of 563.6 g/mol and molecular formula is C27H33NO10S with the chemical structure as below:
8.0 Pharmaceutical particulars
8.1 Incompatibilities
Not applicable.
8.2 Shelf-life
Refer on the pack
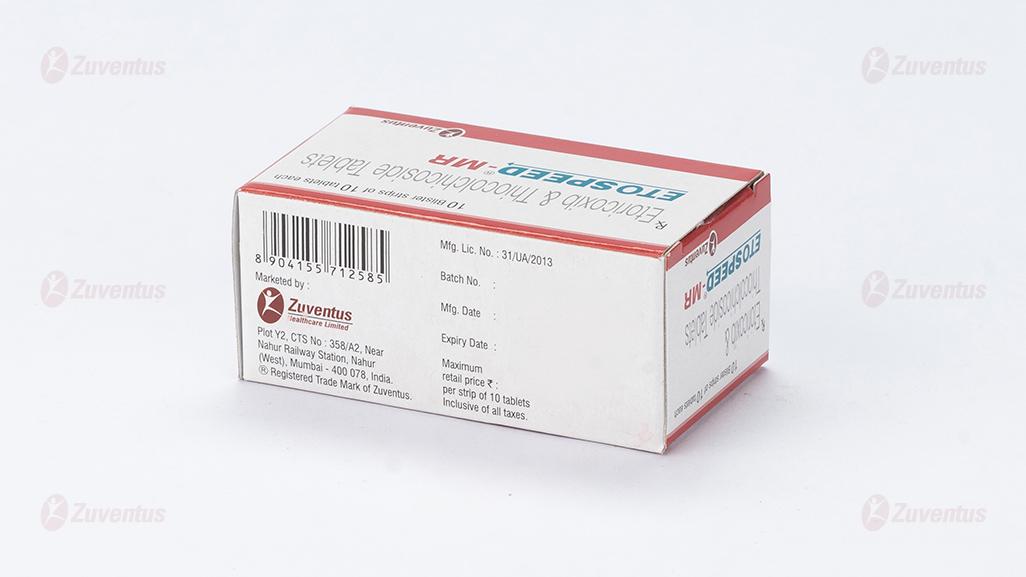
8.3 Packaging information
ETOSPEED-MR is available in blister strip of 10 tablets.
8.4 Storage and handing instructions
Store protected from light & moisture, at a temperature not exceeding 30ºC.
Keep out of reach of children.
9.0 Patient Counselling Information
Patients should be informed of the following information before initiating therapy with ETOSPEED-MR and periodically during the course of ongoing therapy.
Cardiovascular Effects
Patients should be informed that celecoxib may cause serious CV side effects such as MI or stroke, which may result in hospitalization and even death. Patients should be informed of the signs and symptoms of chest pain, shortness of breath, weakness, slurring of speech, and to seek immediate medical advice if they observe any of these signs or symptoms. Patients should be informed that celecoxib can lead to the onset of new hypertension or worsening of pre-existing hypertension, and that etoricoxib may impair the response of some antihypertensive agents. Patients should be instructed on the proper follow up for monitoring of blood pressure.
Gastrointestinal Effects
Patients should be informed that celecoxib can cause gastrointestinal discomfort and more serious side effects, such as ulcers and bleeding, which may result in hospitalization and even death. Patients should be informed of the signs and symptoms of ulcerations and bleeding, and to seek immediate medical advice if they observe any signs or symptoms that are indicative of these disorders, including epigastric pain, dyspepsia, melena, and hematemesis.
Hepatic Effects
Patients should be informed of the warning signs and symptoms of hepatotoxicity (e.g., nausea, fatigue, lethargy, pruritus, jaundice, right upper quadrant tenderness, and "flu-like" symptoms). Patients should be instructed that they should stop therapy and seek immediate medical therapy if these signs and symptoms occur.
Adverse Skin Reactions
Patients should be informed that etoricoxib can cause serious skin side effects such as exfoliative dermatitis, SJS, and TEN, which may result in hospitalizations and even death. Although serious skin reactions may occur without warning, patients should be informed of the signs and symptoms of skin rash and blisters, fever, or other signs of hypersensitivity such as itching, and seek immediate medical advice when observing any indicative signs or symptoms.
Patients should be advised to stop etoricoxib immediately if they develop any type of rash and contact their physician as soon as possible.
Weight Gain and Edema
Long-term administration of NSAIDs including etoricoxib has resulted in renal injury. Patients at greatest risk are those taking diuretics, ACE-inhibitors, angiotensin II antagonists, or with renal or liver dysfunction, heart failure, and the elderly.
Patients should be instructed to promptly report to their physicians signs or symptoms of unexplained weight gain or edema following treatment with etoricoxib.
Anaphylactoid Reactions
Patients should be informed of the signs and symptoms of an anaphylactoid reaction (e.g., difficulty breathing, swelling of the face or throat). Patients should be instructed to seek immediate emergency assistance if they develop any of these signs and symptoms.
Effects During Pregnancy
Patients should be informed that in late pregnancy celecoxib should be avoided because it may cause premature closure of the ductus arteriosus.
Pre-existing Asthma
Patients should be instructed to tell their physicians if they have a history of asthma or aspirin sensitive asthma because the use of NSAIDs in patients with aspirin-sensitive asthma has been associated with severe bronchospasm, which can be fatal. Patients with this form of aspirin sensitivity should be instructed not to take celecoxib. Patients with pre-existing asthma should be instructed to seek immediate medical attention if their asthma worsens after taking etoricoxib.
12.0 Date of revision
July 2024
About Leaflet
This product is available as the above name but will be referred to as ETOSPEED®-MR throughout this leaflet.
Read all of this leaflet carefully before you start taking this medicine because it contains important information for you.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effect not listed in this leaflet. See section 4.
What is in this leaflet
1. What ETOSPEED®-MR is and what' it is used for
2. What you need to know before you take ETOSPEED®-MR
3. How to take ETOSPEED®-MR
4. Possible side effects
5. How to store ETOSPEED®-MR
6. Contents of the pack and other information
1. What ETOSPEED®-MR is and what it is used for
ETOSPEED®-MR is combination of active substance etoricoxib and thiocolchicoside (muscle relaxant).
Etoricoxib is a medication belonging to the class of nonsteroidal anti-inflammatory drugs (NSAIDs). It's primarily used to relieve pain and inflammation in conditions such as osteoarthritis, rheumatoid arthritis, acute gouty arthritis, and other musculoskeletal disorders. Etoricoxib works by inhibiting the enzyme cyclooxygenase-2 (COX-2), which is involved in the production of prostaglandins that cause pain and inflammation.
Thiocolchicoside is primarily used as a skeletal muscle relaxant to alleviate muscle spasms and stiffness associated with various musculoskeletal conditions. Thiocolchicoside is commonly prescribed for the relief of acute and chronic muscle spasms. It helps relax muscles by acting on the central nervous system, specifically by enhancing the activity of gamma-aminobutyric acid (GABA) receptors in the spinal cord. It is used in conditions such as: Low Back Pain- Often prescribed for acute or chronic lower back pain associated with muscle spasms. Cervical Spondylosis: Helps alleviate muscle stiffness and spasms in the neck region due to cervical degenerative changes. Post-Traumatic and Post-Surgical Conditions: Thiocolchicoside may be used to manage muscle spasms and stiffness following trauma or surgery.
ETOSPEED®-MR is commonly used for the acute treatment of musculoskeletal disorders associated with painful muscle spasm in adults.
2. What you need to know before you take ETOSPEED®-MR
Do not take ETOSPEED®-MR:
- If you are allergic (hypersensitive) to etoricoxib or any of the other ingredients of this medicine
- If you are allergic to non-steroidal anti-inflammatory drugs (NSAIDs), including aspirin and COX-2 inhibitors.
- If you have a current stomach ulcer or bleeding in your stomach or intestines
- If you have serious liver disease
- If you have serious kidney disease
- If you are or could be pregnant or are breast-feeding
- If you are under 16 years of age
- If you have inflammatory bowel disease, such as Crohn’s Disease, Ulcerative Colitis, or Colitis
- If you have high blood pressure that has not been controlled by treatment (check with your doctor or nurse if you are not sure whether your blood pressure adequately controlled)
- If your doctor has diagnosed heart problems including heart failure (moderate or severe types), angina (chest pain)
- If you have had a heart attack, bypass surgery, peripheral arterial disease (poor circulation in legs or feet due to narrow or blocked arteries).
- If you have had any kind of stroke (including mini-stroke, transient ischaemic attack). Etoricoxib may slightly increase your risk of heart attack and stroke and this is why it should not be used in those who have already had heart problems or stroke.
If you think any of these are relevant to you, do not take the tablets until you have consulted your doctor.
Warnings and precautions
Talk to your doctor or pharmacist before taking ETOSPEED®-MR if:
- You have a history of stomach bleeding or ulcers.
- You are dehydrated, for example by a prolonged bout of vomiting or diarrhoea.
- You have swelling due to fluid retention.
- You have a history of heart failure, or any other form of heart disease.
- You have a history of high blood pressure. ETOSPEED®-MR can increase blood pressure in some people, especially in high doses, and your doctor will want to check your blood pressure from time to time.
- You have any history of liver or kidney disease.
- You are being treated for an infection. ETOSPEED®-MR can mask or hide a fever, which is a sign of infection.
- You have diabetes, high cholesterol, or are a smoker. These can increase your risk of heart disease.
- You are a woman trying to become pregnant.
- You are over 65 years of age.
If you are not sure if any of the above apply to you, talk to your doctor before taking
ETOSPEED®-MR to see if this medicine is suitable for you.
ETOSPEED®-MR works equally well in older and younger adult patients. If you are over 65 years of age, your doctor will want to appropriately keep a check on you. No dosage adjustment is necessary for patients over 65 years of age.
Children
Do not give this medicine to children.
Other medicines and ETOSPEED®-MR
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines, including medicines obtained without a prescription.
In particular, if you are taking any of the following medicines, your doctor may want to monitor you to check that your medicines are working properly, once you start taking ETOSPEED®-MR:
- Medicines that thin your blood (anticoagulants), such as warfarin
- Rifampicin (an antibiotic)
- Methotrexate (a drug used for suppressing the immune system, used in rheumatoid arthritis)
- Ciclosporin or tacrolimus (drugs used for suppressing the immune system)
- Lithium (a medicine used to treat some types of depression)
- medicines used to help control high blood pressure and heart failure called ACE inhibitors angiotensin receptor blockers, examples include enalapril/ ramipril, and losartan, valsartan
- Diuretics (water tablets)
- Digoxin (a medicine for heart failure and irregular heart rhythm)
- Minoxidil (a drug used to treat high blood pressure)
- Salbutamol tablets or oral solution (a medicine for asthma)
- Birth control pills (the combination may increase your risk of side effects)
- Hormone replacement therapy (the combination may increase your risk of side effects)
- Aspirin, the risk of stomach ulcers is greater if you take ETOSPEED®-MR with aspirin.
- Aspirin for prevention of heart attacks or stroke:
ETOSPEED®-MR can be taken with low-dose aspirin. If you are currently taking low-dose aspirin to prevent heart attacks or stroke, you should not stop taking aspirin until you talk to your doctor - aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs): do not take high dose aspirin or other anti-inflammatory medicines while taking ETOSPEED®-MR. The dose must be reduced in case of presence of diarrhoea following oral administration.
After administration by intramuscular route episodes were observed of vasovagal syncope, thus the patient has to be monitored after being injected.
Post marketing cases of cytolytic hepatitis and cholestatic were reported with Thiocolchicoside.
The serious cases (for example fulminant hepatitis) were observed in patients that had taken FANS or paracetamol at the same time. The patients have to be informed to report any sign of hepatic toxicity.
Thiocolchicoside may precipitate seizures especially in epileptic patients or those at risk of convulsions.
The maximum daily oral dose of 16mg must not be exceeded and must be split in two doses at 12-hour interval.
In case you forget to take a dose take the next dose avoiding taking doses close to each other.
Preclinical studies showed that one of Thiocolcoside metabolites (SL59.0955) induced aneuploidy (i.e. alterations in the number of chromosomes in dividing cells) at concentrations close to human exposure observed at doses 8 mg twice daily per os. Aneuploidy is considered as a risk factor for teratogenicity, embryo/foetotoxicity, spontaneous abortion, and impaired male fertility and a potential risk factor for cancer. As a precautionary measure, use of the product at doses exceeding the recommended dose or long-term use should be avoided. Patients should be carefully informed about the potential risk of a possible pregnancy and about effective contraception measures to be followed.
ETOSPEED®-MR with food and drink
The onset of the effect of ETOSPEED®-MR may be faster when taken without food.
Pregnancy
ETOSPEED®-MR Tablets must not be taken during pregnancy. If you are pregnant or think you could be pregnant, or if you are planning to become pregnant, do not take the tablets. If you become pregnant, stop taking the tablets and consult your doctor. Consult your doctor if you are unsure or need more advice.
Breast-feeding
It is not known if ETOSPEED®-MR is excreted in human milk. If you are breast-feeding, or planning to breast-feed, consult your doctor before taking ETOXIB MR. If you are using ETOSPEED®-MR, you must not breast-feed.
Fertility
ETOSPEED®-MR is not recommended in women attempting to become pregnant.
Driving and using machines
Dizziness and sleepiness have been reported in some patients taking ETOXIB MR.
Do not drive if you experience dizziness or sleepiness.
Do not use any tools or machines if you experience dizziness or sleepiness.
3. How to take ETOSPEED®-MR?
Always take this medicine exactly as your doctor has told you. You should check with your doctor or pharmacist if you are not sure.
Do not take more than the recommended dose for your condition. Your doctor will want to discuss your treatment from time to time. It is important that you use the lowest dose that controls your pain and you should not take ETOSPEED®-MR for longer than necessary.
This is because the risk of heart attacks and strokes might increase after prolonged treatment, especially with high doses.
There are different strengths available for this medicinal product and depending on your disease your, doctor will prescribe the tablet strength that is appropriate for you.
The recommended dose is: One table of ETOSPEED-MR one or two times daily or as prescribed by the healthcare professional depending on the severity of the condition being treated.
Use in children
ETOSPEED-MR is NOT suitable for children.
If you take more ETOSPEED-MR than you should
You should never take more tablets than the doctor recommends. If you do take too many ETOXIB MR Tablets, you should seek medical attention immediately.
If you forget to take ETOSPEED-MR
- If you forget a dose, take it as soon as you remember it. However, if it is nearly time for the next dose, skip the missed dose
- Do not take a double dose to make up for a forgotten dose
If you stop taking ETOSPEED-MR
Do not stop taking Sucralfate Suspension without talking to your doctor.
If you have any further questions on the use of this product, ask your doctor or pharmacist.
4. Possible side effects?
Like all medicines, this medicine can cause side effects, although not everybody gets them. If you develop any of these signs you should stop ETOSPEED-MR and talk to your doctor immediately (see what you need to know before you take ETOSPEED-MR section
- Shortness of breath, chest pains, or ankle swelling appear or if they get worse
- yellowing of the skin and eyes (jaundice) – these are signs of liver problems
- Severe or continual stomach pain or your stools become black
- an allergic reaction- which can include skin problems such as ulcers or blistering, or swelling of the face, lips, tongue, or throat which may cause difficulty in breathing The frequency of possible side effects listed below is defined using the following convention:
The following side effects can occur during treatment with ETOXIB MR:
Very Common: Stomach pain
Common:
- Dry socket (inflammation and pain after a tooth extraction)
- swelling of the legs and/or feet due to fluid retention (oedema)
- Dizziness, headache
- Palpitations (fast or irregular heartbeat), irregular heart rhythm (arrhythmia)
- increased blood pressure
- Wheezing or shortness of breath (bronchospasms)
- Constipation, wind (excessive gas), gastritis (inflammation of the lining of the stomach), Heartburn, diarrhoea, indigestion (dyspepsia)/stomach discomfort, nausea, being sick (vomiting), Inflammation of the oesophagus, mouth ulcers
- Changes in blood tests related to your liver
- Bruising
- Weakness and fatigue, flu-like illness
Uncommon:
- Gastroenteritis (inflammation of the gastrointestinal tract that involves both the stomach and small intestine/stomach flu), upper respiratory infection, urinary tract infection
- changes in laboratory values (decreased number of red blood cells, decreased number of white blood cells, platelets decreased)
- Hypersensitivity (an allergic reaction including hives which may be serious enough to require immediate medical attention)
- Appetite increases or decreases, weight gain
- Anxiety, depression, decreases in mental sharpness; seeing, feeling or hearing thing that are not there (hallucinations)
- Taste alteration, inability to sleep, numbness or tingling, sleepiness • Blurred vision, eye irritation and redness
- ringing in the ears, vertigo (sensation of spinning while remaining still)
- abnormal heart rhythm (atrial fibrillation), fast heart rate, heart failure, feeling of tightness, pressure or heaviness in the chest (angina pectoris), heart attack
- flushing, stroke, mini-stroke (transient ischaemic attack), severe increase in blood pressure, inflammation of the blood vessels
- cough, breathlessness, nose bleed
- stomach or bowel bloating, changes in your bowel habits, dry mouth, stomach ulcer, inflammation of the stomach lining that can become serious and may lead to bleeding, irritable bowel syndrome, inflammation of the pancreas
- swelling of the face, skin rash or itchy skin, redness of the skin
- Muscle cramp/spasm, muscle pain/stiffness
- High levels of potassium in your blood, changes in blood or urine tests relating to your kidney, serious kidney problems
- Chest pain
Rare:
- Angioedema (an allergic reaction with swelling of the face, lips, tongue and/or throat which may Cause difficulty in breathing or swallowing, which may be serious enough to require immediate medical attention)/anaphylactic/anaphylactoid reactions including shock (a serious allergic reaction that requires immediate medical attention)
- Confusion, restlessness
- Liver problems (hepatitis)
- Low blood levels of sodium
- Liver failure, yellowing of the skin and/or eyes (jaundice)
- Severe skin reactions
Disturbances in immunity system
Anaphylactic reactions:
Uncommon: pruritis,
Rare: urticarial
Very rare: hypotension
Not noted: angioeodema and anaphylactic shock after intramuscular administration.
Pathology of the nervous system
Common: drowsiness
Rare: agitation and clouding
Not noted: malaise associated or to a lesser extent vasovagal syncope in the minutes following intramuscular administration, convulsions.
Gastrointestinal pathology
Common: diarrhoea, stomach pain
Uncommon: nausea, vomiting
Rare: heartburn after oral administration
Hepatobiliary pathology
Not noted: cytolytic hepatitis and cholestatic.
Pathology of the skin and subcutaneous tissue
Uncommon: allergic skin reactions
Reporting of side effects
If you get any side effects, talk to your doctor. This includes any possible side effects not listed in this leaflet. You can also report side effects directly: Website: www.zuventus.com and click the tab “Safety Reporting” located on the top of the home page. https://www.zuventus.com/drug-safety-reporting
By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store ETOSPEED-MR.
Store below 30°C. Protect from light & moisture.
Keep all medicine out of reach of children.
6. Contents of the pack and other information
What ETOSPEED-MR contains
Composition:
Each film coated tablet contains:
Etoricoxib IP 60 mg
Thiocolchicoside IP 4 mg
Colours: Red Oxide of Iron & Titanium Dioxide IP
Packaging information
1blister strip of 10 tablets each
Marketing Authorisation Holder
Zuventus Healthcare Limited
Zuventus House Plot No. Y2, CTS No: 358/A2,
near Nahur Railway Station, off Raycon IT Park Road,
Nahur West, Mumbai, Maharashtra 400078
Leaflet revision date (Ref.): 08.07.2024.