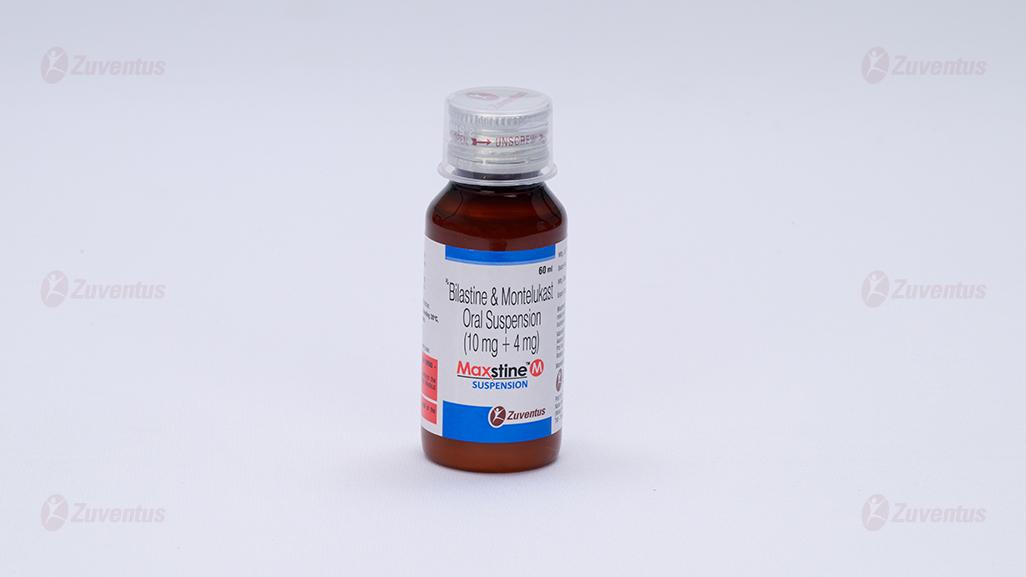
Maxstine M Suspension
Therapy Area
Respiratory
1.0 Generic name
Bilastine & Montelukast Oral Suspension (10 mg + 4 mg)
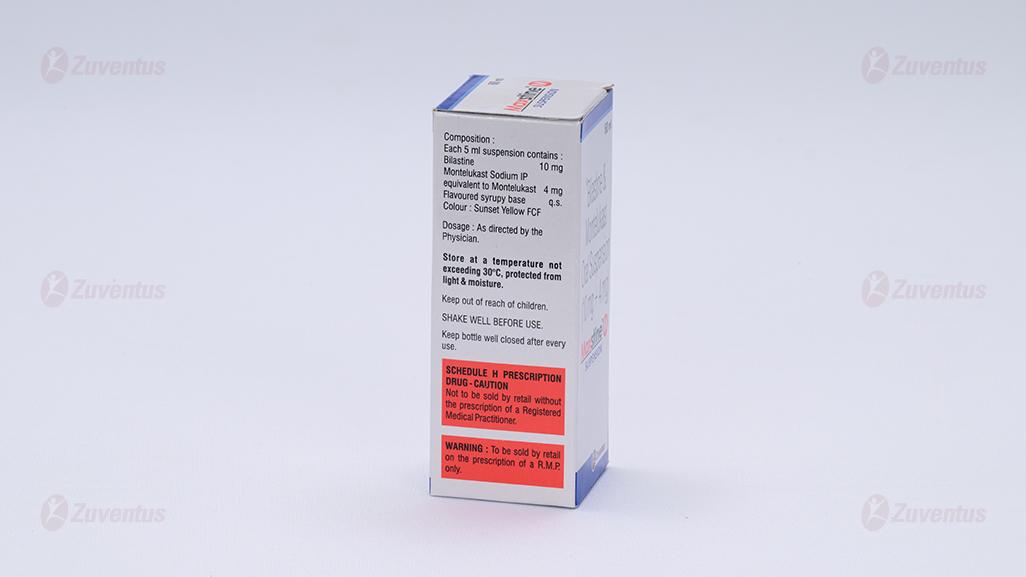
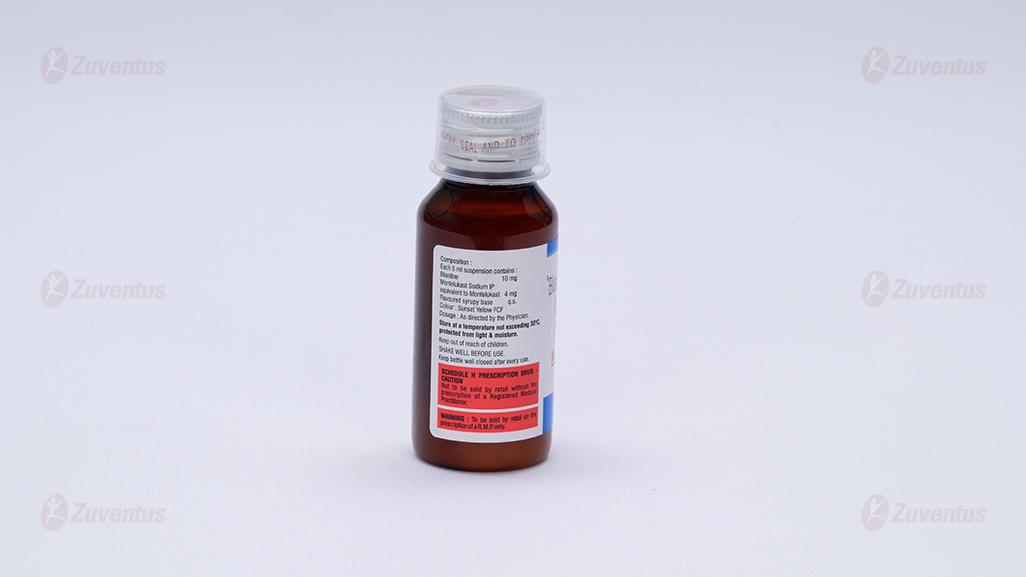
2.0 Qualitative and quantitative composition
Each 5 ml suspension contains :
Bilastine 10 mg
Montelukast Sodium IP
equivalent to Montelukast 4 mg
Flavoured syrupy base q.s.
Colour : Sunset Yellow FCF
3.0 Dosage form and strength
Oral Suspension, Bilastine 10 mg & Montelukast 4 mg
4.0 Clinical particulars
4.1 Therapeutic indication
For treatment of allergic rhinitis in children aged 6 to 11 years (both inclusive) with a body weight of at least 20 kg.
4.2 Posology and method of administration Children (6 to 11 years of age)
5 ml once daily or as directed by the Physician.
Method of administration
For oral use only
The suspension should be taken 1 hour before or 2 hours after intake of food or fruit juice. Shake well before use.
4.3 Contraindications
Known hypersensitivity to Bilastine or Montelukast or any component of the formulation.
History of QT prolongation and/or torsade de pointes, including congenital long QT syndromes.
4.4 Special warnings and precautions for use Cardiovascular
It has been associated with QTc interval prolongation. Drugs that cause QT/QTc prolongation are suspected of increasing the risk of torsade de pointes. Torsade de pointes is a polymorphic ventricular tachyarrhythmia. Generally, the risk of torsade de pointes increases with the magnitude of QT/QTc prolongation produced by the drug. Torsade de pointes may be asymptomatic or experienced by the patient as dizziness, palpitations, syncope, or seizures. If sustained, torsade de pointes can progress to ventricular fibrillation and sudden cardiac death. It should not be used in patients with a history of QTc prolongation and/or torsade de pointes, including congenital long QT syndromes. Particular care should be exercised when administering antihistamines, including Bilastine to patients who are suspected to be at an increased risk of experiencing torsade de pointes during treatment with a QTc-prolonging drug. This includes patients who have a history of cardiac arrhythmias; hypokalemia; hypomagnesaemia; significant bradycardia; family history of sudden cardiac death; concomitant use of other QT/QTc-prolonging drugs. When drugs that prolong the QTc interval are prescribed, healthcare professionals should counsel their patients concerning the nature and implications of the ECG changes, underlying diseases and disorders that are considered to represent risk factors, demonstrated and predicted drug-drug interactions, symptoms suggestive of arrhythmia, risk management strategies, and other information relevant to the use of the drug.
Hepatic
It has not been studied in subjects with hepatic impairment. Since Bilastine is not metabolized and renal clearance is the major route of elimination, hepatic impairment is not expected to increase systemic exposure above the safety margin.
Renal
In subjects with moderate or severe renal impairment co-administration of Bilastine with P glycoprotein inhibitors, such as ketoconazole, erythromycin, cyclosporine, ritonavir or diltiazem, may increase plasma levels of Bilastine and therefore increase the risk of adverse effects. Co administration of Bilastine and P-glycoprotein inhibitors should be avoided in subjects with moderate or severe renal impairment.
Acute asthma
Montelukast is not indicated for use in the reversal of bronchospasm in acute asthma attacks, including status asthmaticus. Patients should be advised to have appropriate rescue medication available. Therapy with Montelukast can be continued during acute exacerbations of asthma. There are no data demonstrating that oral corticosteroids can be reduced when Montelukast is given concomitantly. Patients who have exacerbations of asthma after exercise should have available for rescue a shortacting inhaled beta2-agonist.
Concomitant corticosteroid use
While the dose of inhaled corticosteroid may be reduced gradually under medical supervision, Montelukast should not be abruptly substituted for inhaled or oral corticosteroids.
Aspirin sensitivity
Patients with known aspirin sensitivity should continue avoidance of Aspirin or non-steroidal antiinflammatory agents while taking Montelukast. Although Montelukast is effective in improving airway function in asthmatics with documented aspirin sensitivity, it has not been shown to truncate bronchoconstrictor response to Aspirin and other non-steroidal anti-inflammatory drugs in Aspirinsensitive asthmatic patients.
Eosinophilic conditions
Patients with asthma on therapy with Montelukast may present with systemic eosinophilia, sometimes presenting with clinical features of vasculitis consistent with Churg-Strauss syndrome, a condition which is often treated with systemic corticosteroid therapy. These events usually, but not always, have been associated with the reduction of oral corticosteroid therapy. Physicians should be alert to eosinophilia, vasculitic rash, worsening pulmonary symptoms, cardiac complications, and/or neuropathy presenting in their patients. A causal association between Montelukast and these underlying conditions has not been established. Patients who develop these symptoms should be reassessed and their treatment regimens evaluated.
Neuropsychiatric events
Neuropsychiatric events have been reported in adult, adolescent, and paediatric patients taking Montelukast. Post-marketing reports with Montelukast use include agitation, aggressive behaviour or hostility, anxiousness, depression, disorientation, dream abnormalities, hallucinations, insomnia, irritability, memory impairment, restlessness, somnambulism, suicidal thinking and behaviour (including suicide), tic, and tremor. The clinical details of some post-marketing reports involving Montelukast appear consistent with a drug-induced effect. Patients and prescribers should be alert for neuropsychiatric events. Patients should be instructed to notify their prescriber if these changes occur. Prescribers should carefully evaluate the risks and benefits of continuing treatment with Montelukast if such events occur
4.5 Drugs interactions
Interaction with Ketoconazole or Erythromycin
Concomitant intake of Bilastine and Ketoconazole or Erythromycin increased Bilastine AUC 2-fold and Cmax 2-3 fold. These changes can be explained by interaction with intestinal efflux transporters, since Bilastine is substrate for P-gp and not metabolized. These changes do not appear to affect the safety profile of Bilastine and Ketoconazole or Erythromycin, respectively. Other medicinal products that are substrates or inhibitors of P-gp, such as Cyclosporine, may likewise have the potential to increase plasma concentrations of Bilastine.
Interaction with Diltiazem
Concomitant intake of Bilastine 20 mg and Diltiazem 60 mg increased Cmax of Bilastine by 50%. This effect can be explained by interaction with intestinal efflux transporters, and does not appear to affect the safety profile of Bilastine
Interaction with Lorazepam
Concomitant intake of Bilastine 20 mg and Lorazepam 3 mg for 8 days did not potentiate the depressant CNS effects of Lorazepam
Interaction with Alcohol
The psychomotor performance after concomitant intake of Alcohol and 20 mg Bilastine was similar to that observed after intake of Alcohol and placebo.
Interaction with Grapefruit juice
Concomitant intake of Bilastine and Grapefruit juice decreased Bilastine bioavailability by 30%. This effect may also apply to other fruit juices. The degree of bioavailability decrease may vary between producers and fruits. The mechanism for this interaction is an inhibition of OATP1A2, an uptake transporter for which Bilastine is a substrate. Medicinal products that are substrates or inhibitors of OATP1A2, such as ritonavir or rifampicin, may likewise have the potential to decrease plasma concentrations of Bilastine.
Interaction with food
Food significantly reduces the oral bioavailability of Bilastine by 30%.
Paediatric population
No interaction studies have been performed in children with Bilastine orodispersible suspension. As there is no clinical experience regarding the interaction of Bilastine with other medicinal products, food or fruit juices in children, the results obtained in adult interactions studies should be at present taken into consideration when prescribing Bilastine to children. There are no clinical data in children to state whether changes to the AUC or Cmax due to interactions affect the safety profile of Bilastine.
Montelukast
- Montelukast may be administered with other therapies routinely used in the prophylaxis and chronic treatment of asthma. In drug-interaction studies, the recommended clinical dose of Montelukast did not have clinically important effects on the pharmacokinetics of the following drugs : Theophylline, Prednisone, Prednisolone, Oral contraceptives (Norethindrone 1 mg / Ethinyl Estradiol 35 mcg), Terfenadine, Digoxin, Warfarin, Gemfibrozil, Itraconazole, Thyroid hormones, Sedative hypnotics, Non-steroidal anti-inflammator y agents, Benzodiazepines, Decongestants and Cytochrome P450 (CYP) enzyme inducers.
- In drug interaction studies, the recommended clinical dose of Montelukast did not have clinically important effects on the pharmacokinetics of the following drugs : Oral contraceptives (Norethindrone 1 mg / Ethinyl Estradiol 35 mcg), Terfenadine, Digoxin and Warfarin. Montelukast at doses of ≥ 100 mg daily dosed to pharmacokinetic steady state did not significantly alter the plasma concentrations of either component of an oral contraceptive containing Norethindrone 1 mg / Ethinyl Estradiol 35 mcg. Montelukast at a dose of 10 mg once daily dosed to pharmacokinetic steady state did not change the plasma concentration profile of Terfenadine (a substrate of CYP3A4) or Fexofenadine, the carboxylated metabolite, and did not prolong the QTc interval following co-administration with Terfenadine 60 mg twice daily; did not change the pharmacokinetic profile or urinary excretion of immunoreactive digoxin; did not change the pharmacokinetic profile of Warfarin (primarily a substrate of CYP2C9, 3A4 and 1A2) or influence the effect of a single 30-mg oral dose of warfarin on prothrombin time or the International Normalized Ratio (INR).
- The area under the plasma concentration curve (AUC) for Montelukast was decreased approximately 40% in subjects with co-administration of Phenobarbital. Since Montelukast is metabolised by CYP 3A4, it is reasonable to employ appropriate clinical monitoring in children, when Montelukast is co-administered with inducers of CYP 3A4, such as Phenytoin, Phenobarbital and Rifampicin. • Although additional specific interaction studies were not performed, Montelukast was used concomitantly with a wide range of commonly prescribed drugs in clinical studies without evidence of clinical adverse interactions. These medications included thyroid hormones, sedative hypnotics, non-steroidal anti-inflammatory agents, Benzodiazepines and Decongestants.
- In vitro studies have shown that Montelukast is a potent inhibitor of CYP 2C8. However, data from a clinical drug-drug interaction study involving Montelukast and Rosiglitazone (a probe substrate representative of medicinal products primarily metabolised by CYP- 2C8) demonstrated that Montelukast does not inhibit CYP 2C8 in vivo. Therefore, Montelukast is not anticipated to markedly alter the metabolism of medicinal products metabolised by this enzyme (e.g., Paclitaxel, Rosiglitazone and Repaglinide). Based on further in vitro results in human liver microsomes, therapeutic plasma concentrations of Montelukast do not inhibit CYP 3A4, 2C9, 1A2, 2A6, 2C19, or 2D6.
- In vitro studies have shown that Montelukast is a substrate of CYP 2C8, and to a less significant extent, of 2C9, and 3A4. In a clinical drug-drug interaction study involving Montelukast and Gemfibrozil (an inhibitor of both CYP 2C8 and 2C9) Gemfibrozil increased the systemic exposure of Montelukast by 4.4-fold. No routine dosage adjustment of Montelukast is required upon co-administration with gemfibrozil or other potent inhibitors of CYP 2C8, but the physician should be aware of the potential for an increase in adverse reactions.
- Based on in vitro data, clinically important drug interactions with less potent inhibitors of CYP 2C8 (e.g., Trimethoprim) are not anticipated. Co-administration of Montelukast with Itraconazole, a strong inhibitor of CYP 3A4, resulted in no significant increase in the systemic exposure of Montelukast.
4.6 Use in special populations
Pregnancy
There are no or limited amount of data from the use of Maxstine M in pregnant women. Animal studies do not indicate direct or indirect harmful effects with respect to reproductive toxicity, parturition or postnatal development. As a precautionary measure, it is preferable to avoid the use of Maxstine M during pregnancy. Maxstine M suspension may be used during pregnancy only if it is considered to be clearly essential.
Nursing mothers
The excretion of Maxstine M in milk has not been studied in humans. Available pharmacokinetic data in animals have shown excretion of Maxstine M in milk. A decision on whether to continue/discontinue breast-feeding or to discontinue/abstain from Maxstine therapy must be made taking into account the benefit of breast-feeding for the child and the benefit of Maxstine M therapy for the mother.
Fertility
There are no or limited amount of clinical data. A study in rats did not indicate any negative effect on fertility
4.7 Effects on ability to drive and use machines
Patients should be advised not to drive or use machines until they have established their own response to Maxstine M.
4.8 Undesirable effects
The following adverse reactions have been reported during clinical trials and are ranked using the following frequency :
Infections and infestations
Upper respiratory infection, Oral herpes.
Blood and lymphatic system disorders
Increased bleeding tendency, Thrombocytopenia.
Immune system disorder
Hypersensitivity reactions including anaphylaxis, hepatic eosinophilic infiltration.
Metabolism and nutrition disorders
Increased appetite.
Psychiatric disorders
Anxiety, Insomnia, Dream abnormalities including nightmares, somnambulism, Agitation including
aggressive behaviour or hostility, Depression, Psychomotor hyperactivity (including irritability, restlessness, tremor), Disturbance in attention, Memory impairment, Hallucinations, disorientation, Suicidal thinking and behaviour (suicidality), Obsessive-compulsive symptoms, Dysphemia.
Nervous system disorders
Somnolence, Headache, Dizziness, Drowsiness paraesthesia/hypoesthesia, Seizure.
Ear and labyrinth disorders
Uncommon - Tinnitus, Vertigo.
Cardiac disorders
Right bundle branch block, Sinus arrhythmia, Electrocardiogram QT prolonged, Palpitations.
Respiratory, thoracic and mediastinal disorders
Dyspnoea, Nasal discomfort, Nasal dryness, Epistaxis, Churg-Strauss Syndrome (CSS), Pulmonary eosinophilia.
Gastrointestinal disorders
Nausea, Stomach discomfort, Abdominal pain, Diarrhoea, Dry mouth, Dyspepsia, Gastritis, Vomiting.
Hepatobiliary disorders
Elevated levels of serum transaminases (ALT, AST), Hepatitis (including cholestatic, hepatocellular and mixed-pattern liver injury).
Skin and subcutaneous tissue disorders
Pruritus, rash, Bruising, Urticaria, Angioedema, Erythema nodosum, Erythema multiforme.
Musculoskeletal and connective tissue disorders
Arthralgia, Myalgia including muscle cramps
General disorders and administration site conditions
Fatigue, Thirst, Pyrexia, Asthenia, Malaise, Oedema.
Renal and urinary disorders
Enuresis in children.
Investigations
Increased gammaglutamyltransferase, Increased ALT and AST, Increased blood creatinine, Increased Blood TG, Increased weight.
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via
email to : medico@zuventus.com
4.9 Overdose
Information regarding acute overdose of Bilastine is retrieved from the experience of clinical trials conducted during the development and the post-marketing surveillance. In clinical trials, after administration of Bilastine at doses 10 to 11 times the therapeutic dose (220 mg as single dose or 200 mg/day for 7 days) to 26 adult healthy volunteer’s frequency of treatment emergent adverse events was two times higher than with placebo. The adverse reactions most frequently reported were dizziness, headache and nausea. No serious adverse events and no significant prolongation in the QTc interval were reported. The information collected in the post-marketing surveillance is consistent with that reported in clinical trials. Critical evaluation of Bilastine's multiple dose (100 mg x 4 days) effect on ventricular repolarization by a “thorough QT/QTc cross-over study” involving 30 healthy adult volunteers did not show significant QTc prolongation. In chronic asthma studies, Montelukast has been administered at doses up to 200 mg/day to adult patients for 22 weeks and in short term studies, up to 900 mg/day to patients for approximately one week without clinically important adverse experiences. There have been reports of acute overdose in post-marketing experience and clinical studies with Montelukast. These include reports in adults and children with a dose as high as 1000 mg (approximately 61 mg/kg in a 42-month old child). The clinical and laboratory findings observed were consistent with the safety profile in adults and paediatric patients. In the event of overdose symptomatic and supportive treatment is recommended.
5.0 Pharmacological properties
5.1 Mechanism of action
Bilastine
Bilastine is a non-sedating, long-acting histamine antagonist with selective peripheral H1 receptor antagonist affinity and no affinity for muscarinic receptors. Bilastine inhibited histamine-induced wheal and flare skin reactions for 24 hours following single doses.
Montelukast
The cysteinyl leukotrienes (LTC4, LTD4, LTE4) are potent inflammatory eicosanoids released from various cells including mast cells and eosinophils. These important pro-asthmatic mediators bind to cysteinyl leukotriene (CysLT) receptors. The CysLT type-1 (CysLT1) receptor is found in the human airway (including airway smooth muscle cells and airway macrophages) and on other pro-inflammatory cells (including eosinophils and certain myeloid stem cells). CysLTs have been correlated with the pathophysiology of asthma and allergic rhinitis. In asthma, leukotriene-mediated effects include bronchoconstriction, mucous secretion, vascular permeability, and eosinophil recruitment. In allergic rhinitis, CysLTs are released from the nasal mucosa after allergen exposure during both early- and late-phase reactions and are associated with symptoms of allergic rhinitis. Intranasal challenge with CysLTs has been shown to increase nasal airway resistance and symptoms of nasal obstruction.
5.2 Pharmacodynamic properties
Bilastine
Highly selective for H1 receptors, but has little or no affinity for other receptors. In vitro binding affinity of Maxstine M to H1 receptors was 3-fold higher than that of cetirizine and 5-fold higher than that of Fexofenadine.
Potent and lasting antihistamine action at least similar to cetirizine and superior to Fexofenadine (4 to 11 times).
Rapid onset of action and possesses antihistaminic as well as anti-allergic properties Maxstine M is a “Non- brain-penetrating antihistamine” which has brain H1 receptor occupancy (H1RO) is nearly 0%.
Montelukast
Montelukast is an orally active compound which binds with high affinity and selectivity to the CysLT1 receptor. In clinical studies, Montelukast inhibits bronchoconstriction due to inhaled LTD4 at doses as low as 5 mg. Bronchodilation was observed within 2 hours of oral administration. The bronchodilation effect caused by a β agonist was additive to that caused by Montelukast. Treatment with Montelukast inhibited both early- and late phase bronchoconstriction due to antigen challenge. Montelukast, compared with placebo, decreased peripheral blood eosinophils in adult and paediatric patients. In a separate study, treatment with Montelukast significantly decreased eosinophils in the airways (as measured in sputum) and in peripheral blood while improving clinical asthma control
5.3 Pharmacokinetic properties
Bilastine
Absorption
Bilastine is rapidly absorbed after oral administration with a time to maximum plasma concentration of around 1.3 hours. No accumulation was observed. The mean value of Bilastine oral bioavailability is 61%.
Distribution
In vitro and in vivo studies have shown that Bilastine is a substrate Interaction with Ketoconazole or Erythromycin and Interaction with Diltiazem and OATP Interaction with grapefruit juice. At therapeutic doses Bilastine is 84 - 90% bound to plasma proteins.
Biotransformation
Bilastine did not induce or inhibit activity of CYP450 isoenzymes in in vitro studies.
Elimination
In a mass balance study performed in healthy adult volunteers, after administration of a single dose 14 of 20 mg C-Bilastine, almost 95% of the administered dose was recovered in urine (28.3%) and faeces (66.5%) as unchanged Bilastine, confirming that Bilastine is not significantly metabolized in humans. The mean elimination half-life calculated in healthy volunteers was 14.5 h.
Montelukast
Absorption
Montelukast is rapidly and nearly completely absorbed following oral administration. Peak plasma concentrations of Montelukast occur 2 to 4 hours after oral doses. The mean oral bioavailability is 64% to 73%. The oral bioavailability and Cmax are not influenced by a standard meal. For the 4 mg chewable suspension, the mean Cmax is achieved 2 hours after administration in pediatric patients 2 to 5 years of age in the fasted state.
Distribution
Montelukast is more than 99% bound to plasma proteins. The steady state volume of distribution of Montelukast averages 8 to 11 liters. Studies in rats with radiolabeled Montelukast indicate minimal distribution across the blood-brain barrier. In addition, concentrations of radiolabeled material at 24 hours post dose were minimal in all other tissues.
Metabolism
Montelukast is extensively metabolized in the liver by cytochrome P450 isoenzymes, mainly by CYP2C8 and to a lesser extent by CYP3A4 and CYP2C9. Therapeutic plasma concentrations of Montelukast do not inhibit cytochromes P450 3A4, 2C9, 1A2, 2A6, 2C19, or 2D6. In studies with therapeutic doses, plasma concentrations of metabolites of Montelukast are undetectable at steady state in adults and pediatric patients.
Elimination
The plasma clearance of Montelukast averages 45 ml/min in healthy adults. Montelukast and its metabolites are excreted principally in the faeces via the bile. Elimination Half-life : 2.7 to 5.5 hours. Following an oral dose of radiolabeled Montelukast, 86% of the radioactivity was recovered in 5-day fecal collections and < 0.2% was recovered in urine. Coupled with estimates of Montelukast oral bioavailability, this indicates that Montelukast and its metabolites are excreted almost exclusively via the bile.
6.0 Nonclinical properties
6.1 Animal toxicology or pharmacology
Bilastine
Non-clinical data with Bilastine reveal no special hazard for humans based on conventional studies of safety pharmacology, repeated dose toxicity, genotoxicity and carcinogenic potential. In reproduction toxicity studies effects of Bilastine on the foetus (pre-and post-implantation loss in rats and incomplete ossification of cranial bones, sternebrae and limbs in rabbits) were only observed at maternal toxic doses. The exposure levels at the NOAELs are sufficiently in excess (> 30 fold) to the human exposure at the recommended therapeutic dose. In a lactation study, Bilastine was identified in the milk of nursing rats administered a single oral dose (20 mg/kg). Concentrations of Bilastine in milk were about half of those in maternal plasma. The relevance of those results for humans is unknown. In a fertility study in rats, Bilastine administered orally up to 1000 mg/kg/day did not induce any effect on female and male reproductive organs. Mating, fertility and pregnancy indices were not affected. As seen in a distribution study in rats with determination of drug concentrations by autoradiography, Bilastine does not accumulate in the CNS.
Montelukast
In animal toxicity studies, minor serum biochemical alterations in ALT, glucose, phosphorus and triglycerides were observed which were transient in nature. The signs of toxicity in animals were increased excretion of saliva, gastro-intestinal symptoms, loose stools and ion imbalance. These occurred at dosages which provided > 17-fold the systemic exposure seen at the clinical dosage. In monkeys, the adverse effects appeared at doses from 150 mg/kg/day (> 232-fold the systemic exposure seen at the clinical dose). In animal studies, Montelukast did not affect fertility or reproductive performance at systemic exposure exceeding the clinical systemic exposure by greater than 24-fold. A slight decrease in pup body weight was noted in the female fertility study in rats at 200 mg/kg/day (> 69 fold the clinical systemic exposure). In studies in rabbits, a higher incidence of incomplete ossification, compared with concurrent control animals, was seen at systemic exposure > 24-fold the clinical systemic exposure seen at the clinical dose. No abnormalities were seen in rats. Montelukast has been shown to cross the placental barrier and is excreted in breast milk of animals. No deaths occurred following a single oral administration of Montelukast sodium at doses up to 5000 mg/kg 2 2 in mice and rats (15,000 mg/m and 30,000 mg/m in mice and rats, respectively), the maximum dose tested. This dose is equivalent to 25,000 times the recommended daily adult human dose (based on an adult patient weight of 50 kg). Montelukast was determined not to be phototoxic in mice for UVA, UVB or visible light spectra at doses up to 500 mg/kg/day (approximately > 200-fold based on systemic exposure). Montelukast was neither mutagenic in in vitro and in vivo tests nor tumorigenic in rodent species.
7.0 Description
Bilastine is a novel, benzimidazole-piperidine derivative that is a highly selective second-generation H1 antihistamine. Montelukast sodium, is a selective and orally active leukotriene receptor antagonist that inhibits the cysteinyl leukotriene CysLT1 receptor
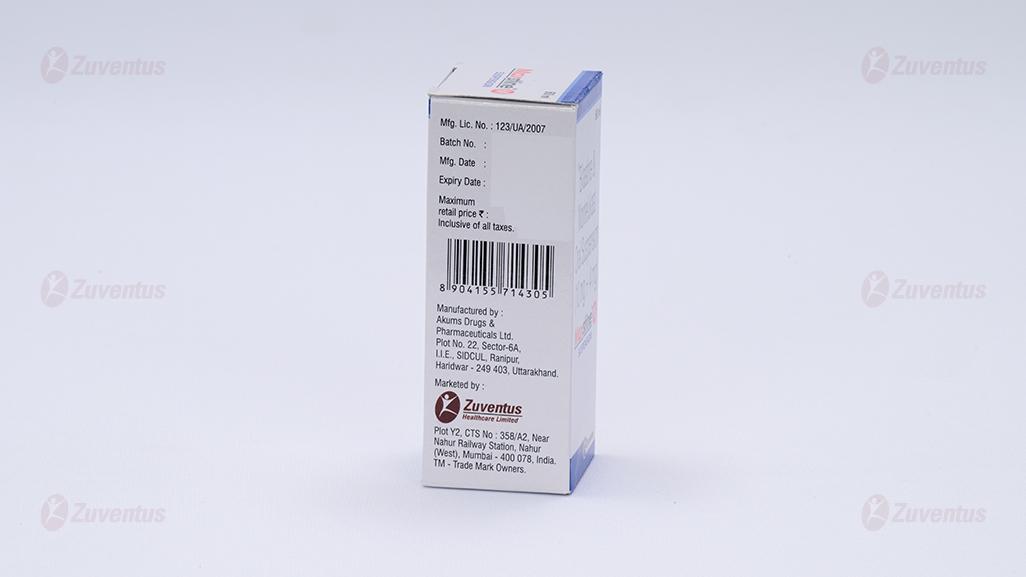
8.0 Pharmaceutical particulars
8.1 Incompatibilities
Not applicable
8.2 Shelf-life
Refer on the pack
8.3 Packaging information
A bottle of 60 ml.
8.4 Storage and handing instructions Store at a temperature not exceeding 30°C, protected from light and moisture.
Keep out of reach of children.
Keep bottle well closed after every use.
9.0 Patient counselling information
- Do not take this medicine, if you are allergic to Bilastine or Montelukast.
- Signs of an allergic reaction include a rash, itching or shortness of breath.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet.
- Be alert for changes in behaviour or new neuropsychiatric symptoms when taking Montelukast sodium. If changes in behaviour are observed, or if new NP symptoms or suicidal thoughts and/or behaviour occur, advise patients to discontinue Montelukast sodium and contact a healthcare provider immediately.
- If you have any further questions, ask your doctor or pharmacist.
12.0 Date of issue
20 October 2022
About Leaflet
Read all of this leaflet carefully before your child starts taking this medicine because it contains important information for you.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for your child. Do not pass it on to others. It may harm them, even if their signs of illness are the same as your child’s.
- If your child gets any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet.
What is in this leaflet?
- What Maxstine™ M suspension is and what it is used for?
- What you need to know before you take Maxstine™ M suspension?
- How to take Maxstine™ M suspension?
- Possible side effects
- How to store Maxstine™ M suspension?
- Contents of the pack and other information
1. What Maxstine™ M suspension is and what it is used for?
Maxstine™ M suspension contains two active substances: bilastine, an antihistamine, and montelukast, a leukotriene receptor antagonist.
Here’s how each works:
When our body has an allergic reaction, inflammatory substances such as leukotrienes and histamine, etc., are released. These substances are produced by the body's immune system in response to allergens.
Bilastine prevents histamine production by inhibiting inflammatory responses mediated by mast cells, basophils, epithelial cells, eosinophils, and lymphocytes. It effectively relieves allergic nasal symptoms such as itching, sneezing, and runny nose (rhinorrhea).
Montelukast targets chemicals called leukotrienes, which cause inflammation in the nasal passages, leading to increased mucus production, swelling of the nasal tissues, and nasal congestion during allergic rhinitis. By blocking these chemicals, Montelukast reduces swelling and symptoms like congestion and inflammation, helping to relieve allergic rhinitis
Maxstine™ M suspension is used to relieve the symptoms of hayfever (sneezing, itchy, runny, blocked-up nose and red and watery eyes) and other forms of allergic rhinitis.
Maxstine™ M is an oral solution is indicated in children aged 6 to 11 years with a body weight of at least 20 kg.
2. What you need to know before you take Maxstine™ M suspension?
Do not use Maxstine™ M suspension:
- if your child is allergic to bilastine, montelukast or any of the other ingredients of this medicine
Warnings and precautions
Talk to your doctor or pharmacist before using Maxstine™ M suspension if your child has moderate or severe renal or hepatic impairment or if your child is taking other medicines (see” Other medicines and Maxstine™ M suspension”).
Various neuropsychiatric events (for example behaviour and mood-related changes, depression and suicidality) have been reported in patients of all ages treated with montelukast (see section 4). If you develop such symptoms while taking montelukast, you should contact your doctor.
Children
Do not give this medicine to children under 6 years of age with a body weight below 20 kg since no sufficient data are available.
Other medicines and Maxstine™ M suspension
Tell your doctor or pharmacist if your child is taking, has recently taken or might take any other medicines, including medicines obtained without a prescription. Some medicines should not be taken together and others may need their doses to be altered when taken together.
Always inform your doctor or pharmacist if your child is using or receiving any of the following medicines in addition to Maxstine™ M suspension:
- Ketoconazole (an antifungal medicine)
- Erythromycin (an antibiotic)
- Diltiazem (to treat angina pectoris – pain or tightness in the chest area)
- Cyclosporine (to reduce the activity of your immune system, thus avoiding transplant rejection or reducing disease activity in autoimmune and allergic disorders, such as psoriasis, atopic dermatitis or rheumatoid arthritis)
- Ritonavir (to treat AIDS)
- Rifampicin (an antibiotic)
- phenobarbital (used for treatment of epilepsy)
- phenytoin (used for treatment of epilepsy)
Maxstine™ M suspension with food, drink and alcohol
The oral solution should not be taken with food or with grapefruit juice or other fruit juices, as this will decrease the effect of bilastine. To avoid this, you can:
- give your child the oral solution and wait for one hour before your child takes food or fruit juice or
- if your child has taken food or fruit juice, wait for two hours before giving him the oral solution.
- Bilastine, at the dose recommended in adults (20 mg), does not increase the drowsiness produced by alcohol.
Pregnancy, breast-feeding and fertility
This medicine is for use in children from 6 to 11 years of age with a body weight of at least 20 kg. However, the following information should be noted regarding the safe use of this medicine. There are no or limited amount of data from the use of bilastine in pregnant women and during breast-feeding and on the effects on fertility.
In case of pregnancy or breast-feeding, or when planning to have a baby, it is recommended to ask to the doctor for advice before taking this medicine. Ask your doctor or pharmacist for advice before taking any medicine.
Driving and using machines
It has been demonstrated that Maxstine™ M suspension does not affect the driving performance in adults. However, the response from each patient to the medicine may be different. Certain side effects (such as dizziness and drowsiness) that have been reported with montelukast may affect some patients’ ability to drive or operate machinery Therefore you should check how this medicine affects your child, before you let your child ride bicycles or drive other vehicles or operate machinery.
3. How to take Maxstine™ M suspension?
Always use this medicine exactly as your doctor or pharmacist has told you. Check with your doctor or pharmacist if you are not sure.
Use in children
The recommended dose in children 6 to 11 years of age with a body weight of at least 20 kg is 5 ml of oral solution once daily for the relief of symptoms of allergic rhinitis.
Do not give this medicine to children under 6 years of age with a body weight below 20 kg since no sufficient data are available
The oral solution is for oral use
- The bottle of oral solution is provided with a child-proof cap and must be opened as follows: press the plastic screw-cap downwards and turn anti-clockwise at the same time
- Fill the cup with 5 ml of oral solution
- Administer directly from the cup
- Wash the cup after use
- You should give the oral solution to your child one hour before or two hours after your child has taken any food or fruit juice.
As the duration of treatment depends on your child’s underlying disease, your physician will determine for how long your child should take Maxstine™ M.
If you use more Maxstine™ M suspension than you should
If your child, or anyone else, use too much of this medicine, tell your doctor immediately or go to the emergency department of your nearest hospital. Please remember to take this medicine pack or this leaflet with you.
If you forget to use Maxstine™ M suspension
If you forget to give your child the daily dose on time, give it on the same day as soon as you remember. Then, give the next dose on the next day at the usual time as prescribed by the doctor. In any case, do not give a double dose to make up for a forgotten one.
If you stop using Maxstine™ M suspension
Generally, there will be no after-effects when treatment with Maxstine™ M suspension is stopped. If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them. If your child experiences symptoms of an allergic reaction the signs of which may include difficulty in breathing, dizziness, collapsing or losing consciousness, swelling of the face, lips, tongue or throat, and/or swelling and redness of the skin, stop giving the medicine and seek urgent medical advice straight away.
Other side effects that may be experienced in children are:
Very common: the following may affect more than 1 in 10 people
- upper respiratory infection
Common: may affect up to 1 in 10 people
- rhinitis (nasal irritation)
- allergic conjunctivitis (eye irritation)
- headache
- stomach pain (abdominal - /upper abdominal pain)
- elevated liver enzymes
- fever
Uncommon: may affect up to 1 in 100 people
- eye irritation
- dizziness
- loss of consciousness
- diarrhoea
- nausea (the feeling of being sick)
- eczema
- urticaria (hives)
- dry mouth, indigestion
- joint or muscle pain, muscle cramps
- bedwetting in children
- weakness/tiredness, feeling unwell, swelling
Rare: the following may affect up to 1 in 1,000 people
- behaviour and mood related changes: disturbance in attention, memory impairment, uncontrolled muscle movements Very rare: the following may affect up to 1 in 10,000 people
- tender red lumps under the skin, most commonly on your shins (erythema nodosum)
- behaviour and mood related changes: obsessive-compulsive symptoms, stuttering
Reporting of side effects
- If you get any side effects, talk to your doctor. This includes any possible side effects not listed in this leaflet. You can also report side effects directly: https://www.zuventus.com/drug-safety-reporting Website: www.zuventus.co.in and click the tab “Safety Reporting” located on the top of the home page.
- By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Maxstine™ M suspension
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date which is stated on the carton and the bottle after EXP. The expiry date refers to the last day of that month
Store at a temperature not exceeding 30°C, protected from light & moisture.
Keep bottle well closed after every use.
Medicines should not be disposed of via wastewater or household waste. Ask your pharmacist on how to dispose of medicines no longer required. These measures will help protect the environment.
6. Contents of the pack and other information
- What Maxstine™ M suspension contains
Each 5 ml suspension contains:
Bilastine IP 10 mg
Montelukast Sodium IP equivalent to Montelukast 4 mg
Flavoured syrupy base q.s.
- What Maxstine™ M suspension looks like and contents of the pack
Maxstine™ M is Sunset Yellow colour oral solution
Each bottle contains 60 ml of oral solution
- Marketing Authorisation Holder and Manufacturer