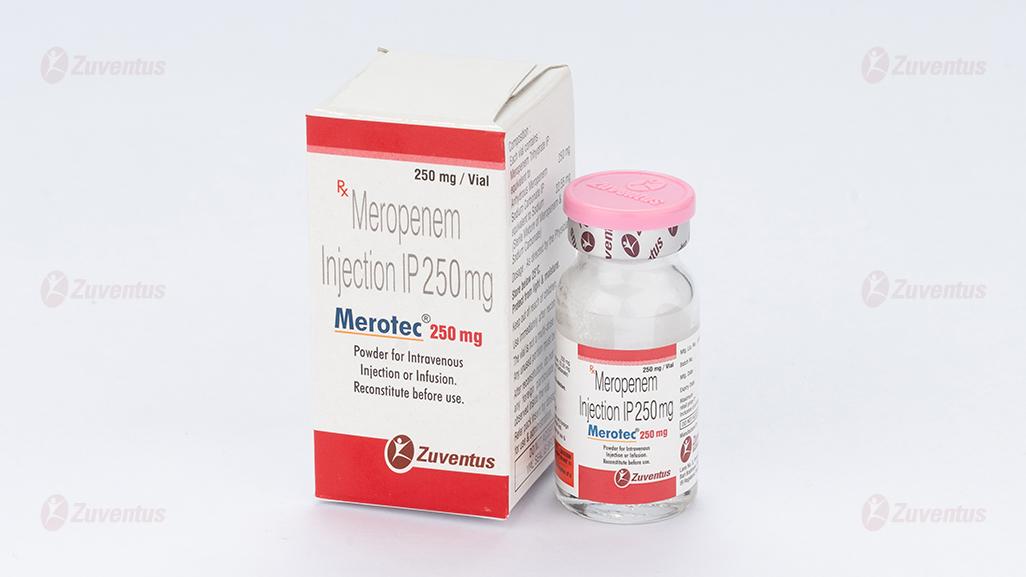
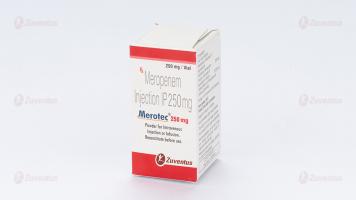
Merotec® 250 mg Injection
Therapy Area
Anti Infective
1.0 Generic Name
Meropenem Injection IP 125 mg / 250 mg / 500 mg / 1 gm / 2 gm
2.0 Qualitative and quantitative composition
Merotec 125 mg
Each vial contains :
Meropenem Trihydrate IP equivalent to Anhydrous Meropenem 125 mg
Sodium Carbonate IP equivalent to Sodium 11.275 mg
(Sterile Mixture of Meropenem & Sodium Carbonate)
This pack contains Sterile Water for Injections IP 5 ml.
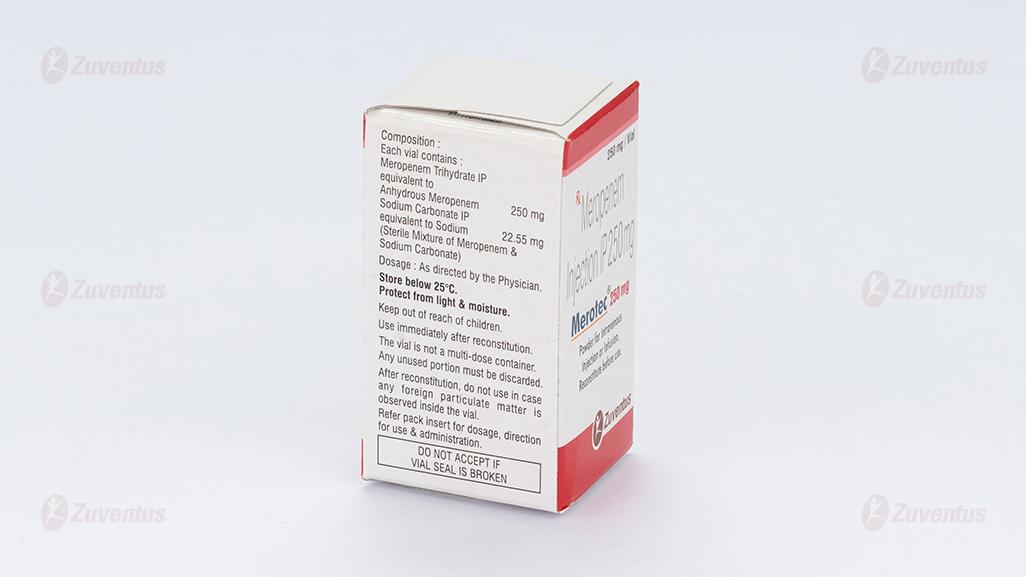
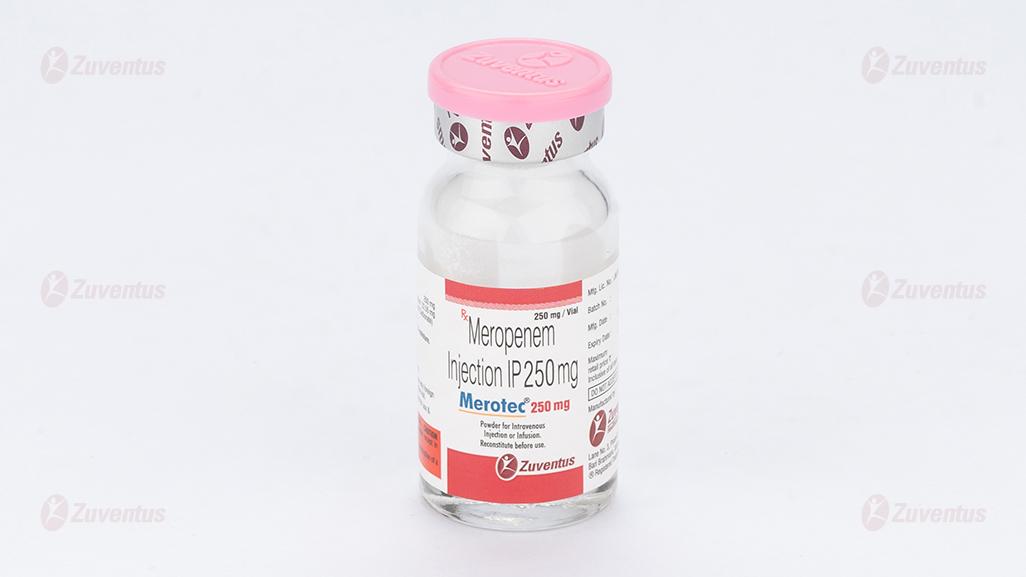
Merotec 250 mg
Each vial contains :
Meropenem Trihydrate IP equivalent to Anhydrous Meropenem 250 mg
Sodium Carbonate IP equivalent to Sodium 22.55 mg
(Sterile Mixture of Meropenem & Sodium Carbonate)
This pack contains Sterile Water for Injections IP 5 ml.
Merotec 500 mg
Each vial contains :
Meropenem Trihydrate IP equivalent to Anhydrous Meropenem 500 mg
Sodium Carbonate IP equivalent to Sodium 45.10 mg
(Sterile Mixture of Meropenem & Sodium Carbonate)
This pack contains Sterile Water for Injections IP 10 ml.
Merotec 1 gm
Each vial contains :
Meropenem Trihydrate IP equivalent to Anhydrous Meropenem 1 gm
Sodium Carbonate IP equivalent to Sodium 90.20 mg
(Sterile Mixture of Meropenem & Sodium Carbonate)
This pack contains Sterile Water for Injections IP 20 ml.
Merotec 2 gm
Each vial contains :
Meropenem Trihydrate IP equivalent to Anhydrous Meropenem 2 gm
Sodium Carbonate IP equivalent to Sodium 180.4 mg
(Sterile Mixture of Meropenem & Sodium Carbonate)
This pack contains Sterile Water for Injections IP 30 ml.
3.0 Dosage form and strength
Powder for Intravenous Injection or Infusion.
125 mg / 250 mg / 500 mg / 1 gm / 2 gm.
4.0 Clinical particulars
4.1 Therapeutic indication
Merotec is indicated for the treatment of adults and children with
- Pneumonia, nosocomial pneumonia,
- Urinary tract infections (UTI),
- Intra-abdominal infection,
- Gynaecological infection (such as endometriaitis),
- Skin & soft tissue infection,
- Meningitis,
- Septicaemia, and
- Empiric treatment of presumed infection in patients with febrile neutropenia
4.2 Posology and method of administration
Posology
The tables below provide general recommendations for dosing.
The dose of meropenem administered and the duration of treatment should take into account the type of infection to be treated, including its severity, and the clinical response.
A dose of up to 2 g three times daily in adults and adolescents and a dose of up to 40 mg/kg three times daily in children may be particularly appropriate when treating some types of infections, such as infections due to less susceptible bacterial species (e.g. Enterobacteriaceae, Pseudomonas aeruginosa, Acinetobacter spp.), or very severe infections.
Additional considerations for dosing are needed when treating patients with renal insufficiency (see further below).
Adults and adolescents
| Infection | Dose to be administered every 8 hours |
| Severe pneumonia including hospital and ventilator-associated pneumonia. | 500 mg or 1g |
| Broncho-pulmonary infections in cystic fibrosis | 2g |
| Complicated urinary tract infections | 500 mg or 1g |
| Complicated intra-abdominal infections | 500 mg or 1g |
| Intra- and post-partum infections | 500 mg or 1g |
| Complicated skin and soft tissue infections | 500 mg or 1g |
| Acute bacterial meningitis | 2g |
| Management of febrile neutropenic patients | 1g |
Meropenem is usually given by intravenous infusion over approximately 15 to 30 minutes. Alternatively, doses up to 1 g can be given as an intravenous bolus injection over approximately 5 minutes. There are limited safety data available to support the administration of a 2 g dose in adults as an intravenous bolus injection.
Renal impairment
The dose for adults and adolescents should be adjusted when creatinine clearance is less than 51 ml/min, as shown below. There are limited data to support the administration of these dose adjustments for a unit dose of 2 g.
| Creatinine clearance (ml/min) | Dose (based on “unit” dose range of 500 mg or 1 g or 2 g, see table above) | Frequency |
| 26-50 | one unit dose | every 12 hours |
| 10-25 | half of one unit dose | every 12 hours |
| <10 | half of one unit dose | every 24 hours |
Meropenem is cleared by haemodialysis and haemofiltration. The required dose should be administered after completion of the haemodialysis cycle.
There are no established dose recommendations for patients receiving peritoneal dialysis.
Hepatic impairment
No dose adjustment is necessary in patients with hepatic impairment.
Dose in elderly patients
No dose adjustment is required for the elderly with normal renal function or creatinine clearance values above 50 ml/min.
Paediatric population
Children under 3 months of age
The safety and efficacy of meropenem in children under 3 months of age have not been established and the optimal dose regimen has not been identified. However, limited pharmacokinetic data suggest that 20 mg/kg every 8 hours may be an appropriate regimen.
Children from 3 months to 11 years of age and up to 50 kg body weight
The recommended dose regimens are shown in the table below :
| Infection | Dose to be administered every 8 hours |
| Severe pneumonia including hospital and ventilator-associated pneumonia | 10 or 20 mg/kg |
| Broncho-pulmonary infections in cystic fibrosis | 40 mg/kg |
| Complicated urinary tract infections; | 10 or 20 mg/kg |
| Complicated intra-abdominal infections | 10 or 20 mg/kg |
| Complicated skin and soft tissue infections | 10 or 20 mg/kg |
| Acute bacterial meningitis | 40 mg/kg |
| Management of febrile neutropenic patients | 20 mg/kg |
Children over 50 kg body weight.
The adult dose should be administered.
There is no experience in children with renal impairment.
Method of administration
Meropenem is usually given by intravenous infusion over approximately 15 to 30 minutes. Alternatively, meropenem doses of up to 20 mg/kg may be given as an intravenous bolus over approximately 5 minutes. There are limited safety data available to support the administration of a 40 mg/kg dose in children as an intravenous bolus injection.
Direction for use : Dissolve the whole content of vial in 5 / 5 / 10 / 20 / 30 ml of sterile water for injections.
4.3 Contraindications
- Hypersensitivity to the active substance or to any of the excipients.
- Hypersensitivity to any other carbapenem antibacterial agent.
- Severe hypersensitivity (e.g. anaphylactic reaction, severe skin reaction) to any other type of beta-lactam antibacterial agent (e.g. penicillins or cephalosporins).
4.4 Special warnings and precautions for use
The selection of meropenem to treat an individual patient should take into account the appropriateness of using a carbapenem antibacterial agent based on factors such as severity of the infection, the prevalence of resistance to other suitable antibacterial agents and the risk of selecting for carbapenem-resistant bacteria.
Hypersensitivity reactions
As with all beta-lactam antibiotics, serious and occasionally fatal hypersensitivity reactions have been reported.
Patients who have a history of hypersensitivity to carbapenems, penicillins or other beta-lactam antibiotics may also be hypersensitive to meropenem. Before initiating therapy with meropenem, careful inquiry should be made concerning previous hypersensitivity reactions to beta-lactam antibiotics.
If a severe allergic reaction occurs, the medicinal product should be discontinued and appropriate measures taken. Severe cutaneous adverse reactions (SCAR), such as StevensJohnson syndrome (SJS), toxic epidermal necrolysis (TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), erythema multiforme (EM) and acute generalised exanthematous pustulosis (AGEP) have been reported in patients receiving meropenem. If signs and symptoms suggestive of these reactions appear, meropenem should be withdrawn immediately and an alternative treatment should be considered.
Antibiotic-associated colitis
Antibiotic-associated colitis and pseudomembranous colitis have been reported with nearly all anti-bacterial agents, including meropenem, and may range in severity from mild to life threatening. Therefore, it is important to consider this diagnosis in patients who present with diarrhoea during or subsequent to the administration of meropenem. Discontinuation of therapy with meropenem and the administration of specific treatment for Clostridium difficile should be considered. Medicinal products that inhibit peristalsis should not be given.
Seizures
Seizures have infrequently been reported during treatment with carbapenems, including meropenem.
Hepatic function monitoring
Hepatic function should be closely monitored during treatment with meropenem due to the risk of hepatic toxicity (hepatic dysfunction with cholestasis and cytolysis). Use in patients with liver disease: patients with pre-existing liver disorders should have liver function monitored during treatment with meropenem. There is no dose adjustment necessary.
Direct antiglobulin test (Coombs test) seroconversion
A positive direct or indirect Coombs test may develop during treatment with meropenem.
Concomitant use with valproic acid/sodium valproate/valpromide
The concomitant use of meropenem and valproic acid/sodium valproate/valpromide is not recommended.
4.5 Drug interaction
No specific medicinal product interaction studies other than probenecid were conducted.
Probenecid competes with meropenem for active tubular secretion and thus inhibits the renal excretion of meropenem with the effect of increasing the elimination half-life and plasma concentration of meropenem. Caution is required, if probenecid is co-administered with meropenem.
The potential effect of meropenem on the protein binding of other medicinal products or metabolism has not been studied. However, the protein binding is so low that no interactions with other compounds would be expected on the basis of this mechanism.
Decreases in blood levels of valproic acid have been reported when it is co-administered with carbapenem agents resulting in a 60-100 % decrease in valproic acid levels in about two days. Due to the rapid onset and the extent of the decrease, co-administration of valproic acid/sodium valproate/valpromide with carbapenem agents is not considered to be manageable and therefore should be avoided.
Oral anti-coagulants
Simultaneous administration of antibiotics with warfarin may augment its anti-coagulant effects. There have been many reports of increases in the anti-coagulant effectsof orally administered anticoagulant agents, including warfarin in patients who are concomitantly receiving antibacterial agents. The riskmay varywith the underlying infection, age and general statusof the patient so that the contribution of the antibiotic to the increase in INR (international normalised ratio) is difficult to assess. It is recommended that the INR should be monitored frequently during and shortly after coadministration of antibioticswith an oral anti-coagulant agent.
Paediatric population
Interaction studies have only been performed in adults.
4.6 Special Population
Pregnancy
There are no or limited amount of data from the use of meropenem in pregnant women. Animal studies do not indicate direct or indirect harmful effects with respect to reproductive toxicity. As a precautionary measure, it is preferable to avoid the use of meropenem during pregnancy.
Breast-feeding
Small amounts of meropenem have been reported to be excreted in human milk. Meropenem should not be used in breast-feeding women unless the potential benefit for the mother justifies the potential risk to the baby.
4.7 Effects on ability to drive and use machines
No studies on the effect on the ability to drive and use machines have been performed. However, when driving or operating machines, it should be taken into account that headache, paraesthesia and convulsions have been reported for meropenem.
4.8 Undesirable effects
Summary of the safety profile
In a review of 4,872 patients with 5,026 meropenem treatment exposures, meropenem-related adverse reactions most frequently reported were diarrhoea (2.3%), rash (1.4%), nausea/vomiting (1.4%) and injection site inflammation (1.1%). The most commonly reported meropenem-related laboratory adverse events were thrombocytosis (1.6%) and increased hepatic enzymes (1.5-4.3%).
Tabulated risk of adverse reactions
In the table below all adverse reactions are listed by system organ class and frequency: ver y common (≥ 1/10); common (≥ 1/100 to <1/10); uncommon (≥ 1/1,000 to <1/100); rare (≥ 1/10,000 to <1/1,000); very rare (< 1/10,000); not known (cannot be estimated from the available data). Within each frequency grouping, undesirable effects are presented in order of decreasing seriousness.

Paediatric population
Meronem is licensed for children over 3 months of age. There is no evidence of an increased risk of any adverse drug reaction in children based on the limited available data. All reports received were consistent with events observed in the adult population.
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via email to : medico@zuventus.com
Website : http://www.zuventus.co.in/safety.aspx
By reporting side effects, you can help provide more information on the safety of this medicine.
4.9 Overdose
Relative overdose may be possible in patients with renal impairment, if the dose is not adjusted. Limited post-marketing experience indicates that if adverse reactions occur following overdose, they are consistent with the adverse reaction profile, are generally mild in severity and resolve on withdrawal or dose reduction. Symptomatic treatments should be considered. In individuals with normal renal function, rapid renal elimination will occur. Haemodialysis will remove meropenem and its metabolite.
5.0 Pharmacological properties
5.1 Mechanism of action
Meropenem exerts its bactericidal activity by inhibiting bacterial cell wall synthesis in Gram-positive and Gram-negative bacteria through binding to penicillin-binding proteins (PBPs).
5.2 Pharmacodynamic properties
Pharmacokinetic / Pharmacodynamic (PK/PD) relationship
Similar to other beta-lactam antibacterial agents, the time that meropenem concentrations exceed the MIC (T>MIC) has been shown to best correlate with efficacy. In preclinical models, meropenem demonstrated activity when plasma concentrations exceeded the MIC of the infecting organisms for approximately 40% of the dosing interval. This target has not been established clinically.
Mechanism of resistance
Bacterial resistance to meropenem may result from: (1) decreased permeability of the outer membrane of Gram-negative bacteria (due to diminished production of porins) (2) reduced affinity of the target PBPs (3) increased expression of efflux pump components, and (4) production of beta-lactamases that can hydrolyse carbapenems.
Localised clusters of infections due to carbapenem-resistant bacteria have been reported in the European Union.
There is no target-based cross-resistance between meropenem and agents of the quinolone, aminoglycoside, macrolide and tetracycline classes. However, bacteria may exhibit resistance to more than one class of antibacterial agents when the mechanism involved include impermeability and/or an efflux pump(s).
The prevalence of acquired resistance may vary geographically and with time for selected species and local information on resistance is desirable, particularly when treating severe infections. As necessary, expert advice should be sought when the local prevalence of resistance is such that the utility of the agent in at least some types of infections is questionable.
The following table of pathogens listed is derived from clinical experience and therapeutic guidelines.
5.3 Pharmacokinetic properties
In healthy subjects the mean plasma half-life is approximately 1 hour; the mean volume of distribution is approximately 0.25 l/kg (11-27 l) and the mean clearance is 287 ml/min at 250 mg falling to 205 ml/min at 2 g. Doses of 500, 1000 and 2000 mg doses infused over 30 minutes give mean Cmax values of approximately 23, 49 and 115 μg/ml respectively, corresponding AUC values were 39.3, 62.3 and 153 μg.h/ml. After infusion over 5 minutes Cmax values are 52 and 112 μg/ml after 500 and 1000 mg doses respectively. When multiple doses are administered 8-hourly to subjects with normal renal function, accumulation of meropenem does not occur.
A study of 12 patients administered meropenem 1000 mg 8 hourly post-surgically for intra-abdominal infections showed a comparable Cmax and half-life to normal subjects but a greater volume of distribution 27 l.
Distribution
The average plasma protein binding of meropenem was approximately 2% and was independent of concentration. After rapid administration (5 minutes or less) the pharmacokinetics are biexponential but this is much less evident after 30 minutes infusion. Meropenem has been shown to penetrate well into several body fluids and tissues: including lung, bronchial secretions, bile, cerebrospinal fluid, gynaecological tissues, skin, fascia, muscle, and peritoneal exudates.
Biotransformation
Meropenem is metabolised by hydrolysis of the beta-lactam ring generating a microbiologically inactive metabolite. In vitro meropenem shows reduced susceptibility to hydrolysis by human dehydropeptidase-I (DHP-I) compared to imipenem and there is no requirement to co-administer a DHP-I inhibitor.
Elimination
Meropenem is primarily excreted unchanged by the kidneys; approximately 70% (50 –75%) of the dose is excreted unchanged within 12 hours. A further 28% is recovered as the microbiologically inactive metabolite. Faecal elimination represents only approximately 2% of the dose. The measured renal clearance and the effect of probenecid show that meropenem undergoes both filtration and tubular secretion.
6.0 Nonclinical properties
6.1 Animal Toxicology or Pharmacology
Animal studies indicate that meropenem is well tolerated by the kidney. Histological evidence of renal tubular damage was seen in mice and dogs only at doses of 2000 mg/kg and above after a single administration and above and in monkeys at 500 mg/kg in a 7-day study.
Meropenem is generally well tolerated by the central nervous system. Effects were seen in acute toxicity studies in rodent at doses exceeding 1000 mg/kg.
The IV LD50 of meropenem in rodents is greater than 2000 mg/kg.
In repeat dose studies of up to 6 months duration, only minor effects were seen including a decrease in red cell parameters in dogs.
There was no evidence of mutagenic potential in a conventional test battery and no evidence of reproductive toxicity including teratogenic potential in studies in rats up to 750 mg/kg and in monkeys up to 360 mg/kg.
There was no evidence of increased sensitivity to meropenem in juveniles compared to adult animals. The intravenous formulation was well tolerated in animal studies.
The sole metabolite of meropenem had a similar profile of toxicity in animal studies.
7.0 Description
Merotec contains meropenem trihydrate. Meropenem trihydrate an antibacterial drug. It acts by inhibiting bacterial cell wall synthesis.
8.0 Pharmaceutical particulars
8.1 Incompatibilities
Not applicable
8.2 Shelf-life
Refer on the pack.
8.3 Packaging information
Merotec 125 mg : A vial of 125 mg with SWFI IP 5 ml.
Merotec 250 mg : A vial of 250 mg with SWFI IP 5 ml.
Merotec 500 mg : A vial of 500 mg with SWFI IP 10 ml.
Merotec 1 gm : A vial of 1 gm with SWFI IP 20 ml.
Merotec 2 gm : A vial of 2 gm with SWFI IP 30 ml.
8.4 Storage and handing instructions
Store below 25°C. Protect from light & moisture.
Keep out of reach of children.
9.0 Patient Counselling Information
- Counsel patients that antibacterial drugs including Meropenem for Injection should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When Meropenem for Injection is prescribed to treat a bacterial infection, tell patients that although it is common to feel better early in the course of therapy, take the medication exactly as directed. Skipping doses or not completing the full course of therapy may (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by Meropenem for Injection or other antibacterial drugs in the future.
- Counsel patients that diarrhea is a common problem caused by antibacterial drugs which usually ends when the antibacterial drug is discontinued. Sometimes after starting treatment with antibacterial drugs, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibacterial drug. If this occurs, patients should contact their physician as soon as possible.
- Counsel patients to inform their physician if they are taking valproic acid or divalproex sodium. Valproic acid concentrations in the blood may drop below the therapeutic range upon co-administration with Meropenem for Injection. If treatment with Meropenem for Injection is necessary and continued, alternative or supplemental anti-convulsant medication to prevent and/or treat seizures may be needed.
- Patients receiving Meropenem for Injection on an outpatient basis may develop adverse events such as seizures, headaches and/or paresthesias that could interfere with mental alertness and/or cause motor impairment. Until it is reasonably well established that Meropenem for Injection is well tolerated, patients should not operate machinery or motorized vehicles.
12.0 Date of revision
10 October 2023
About leaflet
Read all of this leaflet carefully before you start taking this medicine because it contains important information for you.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor or pharmacist or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist or nurse. This includes any possible side effects not listed in this leaflet.
What is in this leaflet:
1. What MEROTEC® is and what it is used for
2. What you need to know before you take MEROTEC®
3. How to take MEROTEC®
4. Possible side effects
5. How to store MEROTEC®
6. Contents of the pack and other information
1. What MEROTEC® is and what it is used for
MEROTEC® contains the active substance meropenem and belongs to a group of medicines called carbapenem antibiotics. It works by killing bacteria, which can cause serious infections.
MEROTEC® is used to treat the following in adults and children aged 3 months and older:
- Infection affecting the lungs (pneumonia)
- Lung and bronchial infections in patients suffering from cystic fibrosis
- Complicated urinary tract infections
- Complicated infections in the abdomen
- Infections that you can catch during or after the delivery
- Complicated skin and soft tissue infections
- Acute bacterial infection of the brain (meningitis)
MEROTEC® may be used in the management of neutropenic patients with fever that is suspected to be due to a bacterial infection.
Meropenem may be used to treat bacterial infection of the blood which might be associated with a type of infection mentioned above.
2. What you need to know before you take MEROTEC®
Do not take MEROTEC®, if
- you are allergic (hypersensitive) to meropenem or any of the other ingredients of this medicine.
- you are allergic (hypersensitive) to other antibiotics such as penicillins, cephalosporins, or carbapenems as you may also be allergic to meropenem.
Warnings and precautions
Talk to your doctor, pharmacist, or nurse before using MEROTEC® if:
- you have health problems, such as liver or kidney problems.
- you have had severe diarrhea after taking other antibiotics.
You may develop a positive test (Coombs test) which indicates the presence of antibodies that may destroy red blood cells. Your doctor will discuss this with you.
You may develop signs and symptoms of severe skin reactions. If this happens talk to your doctor or nurse immediately so that they can treat the symptoms.
If you are not sure if any of the above applies to you, talk to your doctor or nurse before using MEROTEC®.
Other medicines and MEROTEC®
Tell your doctor, pharmacist or nurse if you are taking, have recently taken or might take any other medicines. This is because MEROTEC® can affect the way some medicines work and some medicines can have an effect on MEROTEC®.
In particular, tell your doctor, pharmacist or nurse if you are taking any of the following medicines:
- Probenecid (used to treat gout).
- Valproic acid/sodium valproate/valpromide (used to treat epilepsy).
- MEROTEC® should not be used because it may decrease the effect of sodium valproate. Oral anti-coagulant agent (used to treat or prevent blood clots).
Pregnancy and breast-feeding
If you are pregnant or breastfeeding, think you may be pregnant, or planning to have a baby, ask your doctor or pharmacist for advice before using this medicine. It is preferable to avoid the use of Meropenem during pregnancy. Your doctor will decide whether you should use MEROTEC®.
It is important that you tell your doctor if you are breast-feeding or if you intend to breast-feed before receiving meropenem. Small amounts of this medicine may pass into the breast milk. Therefore, your doctor will decide whether you should use MEROTEC® while breast-feeding.
Driving and using machines
No studies on the effect on the ability to drive and use machines have been performed.
MEROTEC® has been associated with headache and tingling or pricking skin (paraesthesia).
Any of these side effects could affect your ability to drive or operate machines.
MEROTEC® may cause involuntary muscle movements which may cause the person's body to shake rapidly and uncontrollably (convulsions). This is usually accompanied by a loss of consciousness. Do not drive or use machines if you experience this side effect.
MEROTEC® contains sodium
MEROTEC® 1 g: This medicine contains 90 mg sodium (the main component of cooking/table salt) in each 1 g dose. This is equivalent to 4.5% of the recommended maximum daily dietary intake of sodium for an adult.
If you have a condition that requires you to monitor your sodium intake, please inform your doctor, pharmacist, or nurse.
3. How to use MEROTEC®
Always use this medicine exactly as your doctor, pharmacist or nurse has told you. Check with your doctor, pharmacist or nurse if you are not sure.
Use in adults
- The dose depends on the type of infection that you have, where the infection is in the body, and how serious the infection is. Your doctor will decide on the dose that you need.
- The dose for adults is usually between 500 mg (milligrams) and 2 g (gram). You will usually receive a dose every 8 hours. However, you may receive a dose less often if your kidneys do not work very well.
Use in children and adolescents
- The dose for children over 3 months old and up to 12 years of age is decided using the age and weight of the child. The usual dose is between 10 mg and 40 mg of MEROTEC® for each kilogram (kg) that the child weighs. A dose is usually given every 8 hours. Children who weigh over 50 kg will be given an adult dose.
How to use MEROTEC®
- MEROTEC® will be given to you as an injection or infusion into a large vein.
- Your doctor or nurse will normally give MEROTEC® to you.
- However, some patients, parents and carers are trained to give MEROTEC® at home. Instructions for doing this are provided in this leaflet. Always use MEROTEC® exactly as your doctor has told you. You should check with your doctor if you are not sure.
- Your injection should not be mixed with or added to solutions that contain other medicines.
- The injection may take about 5 minutes or between 15 and 30 minutes. Your doctor will tell you how to give MEROTEC®.
- You should normally have your injections at the same times each day.
If you use more MEROTEC® than you should
If you accidentally use more than your prescribed dose, contact your doctor or nearest hospital
straight away.
If you forget to use MEROTEC®
If you miss an injection, you should have it as soon as possible. However, if it is almost time for your next injection, skip the missed injection. Do not have a double dose (two injections at the same time) to make up for a forgotten dose.
If you stop using MEROTEC®
Do not stop having MEROTEC® until your doctor tells you to.
If you have any further questions on the use of this medicine, ask your doctor, pharmacist or nurse.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Severe allergic reactions
If you have any of these signs and symptoms, tell your doctor or nurse straight away. You may need urgent medical treatment. The signs and symptoms may include a sudden onset of:
- Severe rash, itching or hives on the skin.
- Swelling of the face, lips, tongue or other parts of the body.
- Shortness of breath, wheezing or trouble breathing.
- Serious skin reactions which include
- Serious hypersensitivity reactions involving fever, skin rash, and changes in the blood tests that check how the liver is working (increased levels of liver enzymes) and an increase in a type of white blood cell (eosinophilia) and enlarged lymph nodes. These may be signs of a multi-organ sensitivity disorder known as DRESS syndrome.
- Severe red scaly rash, skin bumps that contain pus, blisters or peeling of skin, which may be associated with a high fever and joint pains.
- Severe skin rashes that can appear as reddish circular patches often with central blisters on the trunk, skin peeling, ulcers of mouth, throat, nose, genitals and eyes and can be preceded by fever and flu-like symptoms (Stevens-Johnson syndrome) or a more severe form (toxic epidermal necrolysis).
Damage to red blood cells (not known)
The signs include:
- Being breathless when you do not expect it.
- Red or brown urine.
If you notice any of the above, see a doctor straight away.
Other possible side effects:
Common (may affect up to 1 in 10 people)
- Abdominal (stomach) pain.
- Feeling sick (nausea).
- Being sick (vomiting).
- Diarrhoea.
- Headache.
- Skin rash, itchy skin.
- Pain and inflammation.
- Increased numbers of platelets in your blood (shown in a blood test).
- Changes in blood tests, including tests that show how well your liver is working.
Uncommon (may affect up to 1 in 100 people)
- Changes in your blood. These include reduced numbers of platelets (which may make you bruise more easily), increased numbers of some white blood cells, decreased numbers of other white cells and increased amounts of a substance called ‘bilirubin’.
- Your doctor may do blood tests from time to time.
- Changes in blood tests, including tests that show how well your kidney is working.
- A tingling feeling (pins and needles).
- Infections of the mouth or the vagina that are caused by a fungus (thrush).
- Inflammation of the bowel with diarrhoea.
- Sore veins where MEROTEC® is injected.
- Other changes in your blood. The symptoms include frequent infections, high temperature and sore throat. Your doctor may do blood tests from time to time.
Rare (may affect up to 1 in 1,000 people)
- Fits (convulsions).
- Acute disorientation and confusion (delirium).
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly: Website: www.zuventus.co.in and click the tab “Safety Reporting” located on the top right end of the home page.
By reporting side effects, you can help provide more information on the safety of this medicine.
You can also report the side effect with the help of your treating physician.
5. How to store MEROTEC®
Keep this medicine out of the sight and reach of children
Do not store above 30°C.
Do not use this medicine after the expiry date which is stated on the label and carton after EXP. The expiry date refers to the last day of that month.
Injection
After reconstitution: The reconstituted solutions for intravenous injection should be used immediately. The time interval between the beginning of reconstitution and the end of intravenous injection should not exceed:
- 3 hours when stored at up to 25°C;
- 12 hours when stored under refrigerated conditions (2-8°C).
Infusion
After reconstitution: The reconstituted solutions for intravenous infusion should be used immediately. The time interval between the beginning of reconstitution and the end of intravenous infusion should not exceed:
- 3 hours when stored at up to 25°C when MEROTEC® is dissolved in sodium chloride;
- 24 hours when stored under refrigerated conditions (2-8°C) when MEROTEC® is dissolved in sodium chloride;
- when MEROTEC® is dissolved in dextrose the solution should be used immediately.
From a microbiological point of view, unless the method of opening/reconstitution/dilution precludes the risk of microbiological contamination, the product should be used immediately. If not used immediately in-use storage times and conditions are the responsibility of the user.
Do not freeze the reconstituted solution.
Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help to protect the environment.
6. Contents of the pack and other information
Merotec 125 mg: A vial of 125 mg Meropenem with SWFI IP 5 ml.
Merotec 250 mg: A vial of 250 mg Meropenem with SWFI IP 5 ml.
Merotec 500 mg: A vial of 500 mg Meropenem with SWFI IP 10 ml.
Merotec 1 gm: A vial of 1 gm Meropenem with SWFI IP 20 ml.
Merotec 2 gm: A vial of 2 gm Meropenem with SWFI IP 30 ml.