Olbet CT 20 Tablet
Therapy Area
Cardiology
1.0 Generic Name
Olmesartan Medoxomil and Chlorthalidone tablets 20mg/12.5mg, 40mg/12.5mg
2.0 Qualitative and quantitative composition
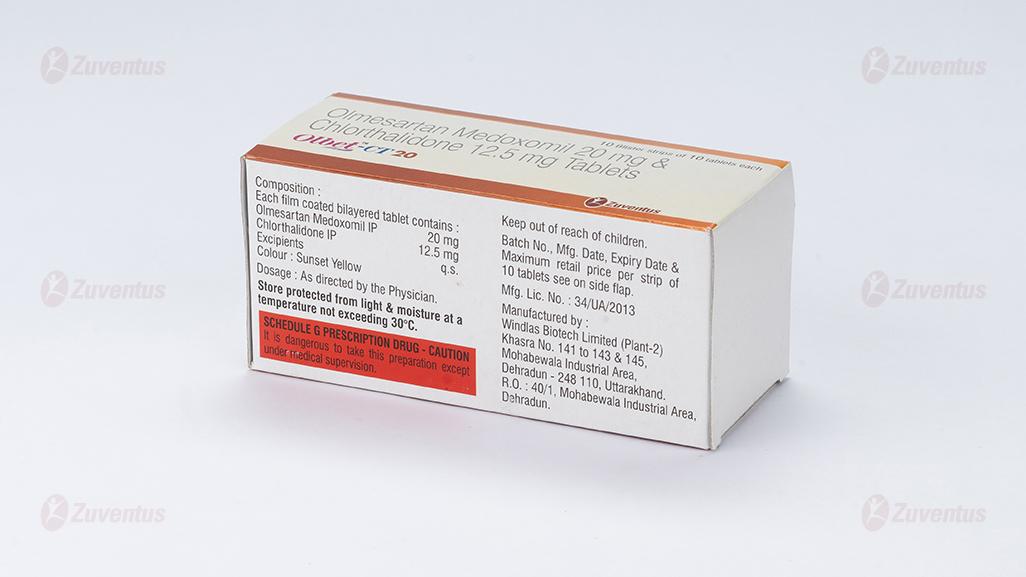
Olbet-CT 20 Tablets
Each film coated bilayered tablets contains:
Olmesartan Medoxomil IP ………. 20mg
Chlorthalidone IP …………………………..12.5 mg
Excipients……………………………………..q.s.
Olbet-CT 40 Tablets
Each film coated bilayered tablets contains:
Olmesartan Medoxomil IP ………. 40mg
Chlorthalidone IP ………………………..12.5 mg
Excipients……………………………………..q.s.
3.0 Dosage form and strength
Film-coated tablet.
4.0 Clinical particulars
4.1 Therapeutic Indication
For the treatment of essential hypertension
4.2 Posology and method of administration
The dose of Olbet-CT is one tablet once daily.
Renal impairment
The maximum dose in patients with mild to moderate renal impairment (creatinine clearance of 20-60 ml/min) is 20 mg olmesartan medoxomil once daily, owing to limited experience of higher dosages in this patient group.
Olbet-CT is not recommended in patients with severe renal failure.
Hepatic impairment
Mild hepatic impairment:
No dose adjustment. Should be used with caution due to the chlorthalidone component, as in patients with impaired hepatic function or progressive liver disease, minor alterations in fluid and electrolyte balance may precipitate hepatic coma.
Moderate hepatic impairment:
An initial dose of 10 mg olmesartan medoxomil once daily is recommended and the maximum dose should not exceed 20 mg once daily. Close monitoring of blood pressure and renal function is advised in hepatically-impaired patients who are already receiving diuretics and/or other antihypertensive agents. Should be used with caution.
Severe hepatic impairment:
NOT recommended in this patient group.
Olmesartan medoxomil should not be used in patients with biliary obstruction.
Elderly patients
No adjustment of dosage is generally required in elderly people. If up-titration of Olmesartan medoxomil to the maximum dose of 40 mg daily is required, blood pressure should be closely monitored.
Paediatric population
Safety and effectiveness of Olbet CT in children have not been established.
4.3 Contraindications
- Hypersensitivity to Olmesartan medoxomil, chlorthalidone or other sulfonamide-derived drugs
- Pregnancy
- Biliary obstruction
- The concomitant use of Olmesartan Tablets with aliskiren-containing products is contraindicated in patients with diabetes mellitus or renal impairment (GFR < 60 ml/min/1.73 m2)
- Anuria
4.4 Special warnings and precautions for use
Olmesartan medoxomil
Intravascular volume depletion
Symptomatic hypotension, especially after the first dose, may occur in patients who are volume and/or sodium depleted by vigorous diuretic therapy, dietary salt restriction, diarrhoea or vomiting. Such conditions should be corrected before the administration of olmesartan medoxomil.
Other conditions with stimulation of the renin-angiotensin-aldosterone system
In patients whose vascular tone and renal function depend predominantly on the activity of the renin-angiotensin-aldosterone system (e.g. patients with severe congestive heart failure or underlying renal disease, including renal artery stenosis), treatment with other drugs that affect this system has been associated with acute hypotension, azotaemia, oliguria or, rarely, acute renal failure. The possibility of similar effects cannot be excluded with angiotensin II receptor antagonists.
Renovascular hypertension
There is an increased risk of severe hypotension and renal insufficiency when patients with bilateral renal artery stenosis or stenosis of the artery to a single functioning kidney are treated with medicinal products that affect the renin-angiotensin-aldosterone system.
Renal impairment and kidney transplantation
When olmesartan medoxomil is used in patients with impaired renal function, periodic monitoring of serum potassium and creatinine levels is recommended. Use of olmesartan medoxomil is not recommended in patients with severe renal impairment (creatinine clearance < 20 ml/min) (see sections 4.2 and 5.2). There is no experience of the administration of olmesartan medoxomil in patients with a recent kidney transplant or in patients with end-stage renal impairment (i.e. creatinine clearance < 12 ml/min).
Hepatic impairment
There is no experience in patients with severe hepatic impairment and therefore use of olmesartan medoxomil in this patient group is not recommended (see section 4.2 for dosage recommendations in patients with mild or moderate hepatic impairment).
Hyperkalaemia
The use of medicinal products that affect the renin-angiotensin-aldosterone system may cause hyperkalaemia.
The risk, that may be fatal, is increased in elderly, in patients with renal insufficiency and in diabetic patients, in patients concomitantly treated with other medicinal products that may increase potassium levels, and/or in patients with intercurrent events.
Before considering the concomitant use of medicinal products that affect the renin-angiotensin-aldosterone system, the benefit risk ratio should be evaluated and other alternatives considered. (see also below section “Dual blockade of the renin-angiotensin-aldosterone system (RAAS)”).
The main risk factors for hyperkalaemia to be considered are:
-Diabetes, renal impairment, age (> 70 years)
-Combination with one or more other medicinal products that affect the renin-angiotensin-aldosterone system and/or potassium supplements. Some medicinal products or therapeutic class of medicinal products may provoke a hyperkalaemia: salt substitutes containing potassium, potassium-sparing diuretics, ACE inhibitors, angiotensin II receptors antagonists, non steroidal anti-inflammatory drugs (including selective COX-2 inhibitors), heparin, immunosuppressor as ciclosporin or tacrolimus, trimethoprim
-Intercurrent events, in particular dehydration, acute cardiac decompensation, metabolic acidosis, worsening of renal function, sudden worsening of the renal condition (e.g. infectious diseases), cellular lysis (e.g. acute limb ischemia, rhabdomyolysis, extended trauma).
Close-monitoring of serum potassium in at risk patients is recommended
Dual blockade of the renin-angiotensin-aldosterone system (RAAS)
There is evidence that the concomitant use of ACE-inhibitors, angiotensin II receptor blockers or aliskiren increases the risk of hypotension, hyperkalaemia and decreased renal function (including acute renal failure). Dual blockade of RAAS through the combined use of ACE-inhibitors, angiotensin II receptor blockers or aliskiren is therefore not recommended.
If dual blockade therapy is considered absolutely necessary, this should only occur under specialist supervision and subject to frequent close monitoring of renal function, electrolytes and blood pressure.
ACE-inhibitors and angiotensin II receptor blockers should not be used concomitantly in patients with diabetic nephropathy.
Lithium
As with other angiotensin-II receptor antagonists, the combination of lithium and olmesartan medoxomil is not recommended.
Aortic or mitral valve stenosis; obstructive hypertrophic cardiomyopathy
As with other vasodilators, special caution is indicated in patients suffering from aortic or mitral valve stenosis, or obstructive hypertrophic cardiomyopathy.
Primary aldosteronism
Patients with primary aldosteronism generally will not respond to antihypertensive drugs acting through inhibition of the renin-angiotensin system. Therefore, the use of olmesartan medoxomil is not recommended in such patients.
Sprue-like enteropathy
In very rare cases severe, chronic diarrhoea with substantial weight loss has been reported in patients taking olmesartan few months to years after drug initiation, possibly caused by a localized delayed hypersensitivity reaction. Intestinal biopsies of patients often demonstrated villous atrophy. If a patient develops these symptoms during treatment with olmesartan, and in the absence of other apparent etiologies, olmesartan treatment should be immediately discontinued and should not be restarted. If diarrhoea does not improve during the week after the discontinuation, further specialist (e.g. a gastro-enterologist) advice should be considered.
Chlorthalidone
Hypotension
Chlorthalidone may cause symptomatic hypotension. Patients with impaired sympathetic response, volume-depletion or who are salt restricted may be at increased risk for developing hypotension. If hypotension occurs, place the patient in the supine position and, if necessary, give intravenous normal saline. A transient hypotensive response is not a contraindication to further treatment, which usually can be continued without difficulty once the blood pressure has stabilized.
Impaired Renal Function
Changes in renal function including acute renal failure can be caused by diuretics. Patients with chronic kidney disease, heart failure, or volume depletion may be at particular risk of developing acute renal failure on Chlorthalidone. Monitor renal function periodically. Consider withholding or discontinuing therapy in patients who develop a clinically significant decrease in renal function on Chlorthalidone.
Electrolyte Abnormalities
Chlorthalidone can cause hypokalemia, hyponatremia, hypochloremic alkalosis, and hypomagnesemia.
Hypomagnesemia can result in hypokalemia which appears difficult to treat despite potassium repletion. Monitor serum electrolytes periodically.
If hypokalemia is accompanied by clinical signs (e.g., muscular weakness, paresis, or ECG alterations),
Chlorthalidone should be discontinued. Correction of hypokalemia and any coexisting hypomagnesemia is recommended prior to the initiation of thiazides.
Metabolic Disturbances
Chlorthalidone may alter glucose tolerance.
Chlorthalidone may raise serum levels of cholesterol and triglycerides.
Chlorthalidone may raise the serum uric acid level due to reduced clearance of uric acid and may cause or exacerbate hyperuricemia and precipitate gout in susceptible patients.
Chlorthalidone decreases urinary calcium excretion and may cause elevations of serum calcium. Monitor calcium levels in patients with hypercalcemia receiving Chlorthalidone
4.5 Drugs interactions
Olmesartan medoxomil
Other antihypertensive medications:
The blood pressure lowering effect of olmesartan medoxomil can be increased by concomitant use of other antihypertensive medications.
ACE-inhibitors, angiotensin II receptor blockers or aliskiren
Clinical trial data has shown that dual blockade of the renin-angiotensin-aldosterone-system (RAAS) through the combined use of ACE-inhibitors, angiotensin II receptor blockers or aliskiren is associated with a higher frequency of adverse events such as hypotension, hyperkalaemia and decreased renal function (including acute renal failure) compared to the use of a single RAAS-acting agent
Potassium supplements and potassium sparing diuretics:
Based on experience with the use of other drugs that affect the renin-angiotensin system, concomitant use of potassium-sparing diuretics, potassium supplements, salt substitutes containing potassium or other drugs that may increase serum potassium levels (e.g. heparin) may lead to increases in serum potassium. Such concomitant use is therefore not recommended.
Non-steroidal anti-inflammatory drugs (NSAIDs):
NSAIDs (including acetylsalicylic acid at doses> 3 g/day and also COX-2 inhibitors) and angiotensin II receptor antagonists may act synergistically by decreasing glomerular filtration. The risk of the concomitant use of NSAIDs and angiotensin II antagonists is the occurrence of acute renal failure. Monitoring of renal function at the beginning of treatment should be recommended as well as regular hydration of the patient.
Additionally, concomitant treatment can reduce the antihypertensive effect of angiotensin II receptor antagonists, leading to their partial loss of efficacy.
Bile acid sequestering agent colesevelam
Concurrent administration of the bile acid sequestering agent colesevelam hydrochloride reduces the systemic exposure and peak plasma concentration of olmesartan and reduces t1/2. Administration of olmesartan medoxomil at least 4 hours prior to colesevelam hydrochloride decreased the drug interaction effect. Administering olmesartan medoxomil at least 4 hours before the colesevelam hydrochloride dose should be considered.
Other compounds:
After treatment with antacid (aluminium magnesium hydroxide), a modest reduction in bioavailability of olmesartan was observed. Coadministration of warfarin and digoxin had no effect on the pharmacokinetics of olmesartan.
Effects of olmesartan medoxomil on other medicinal products:
Lithium:
Reversible increases in serum lithium concentrations and toxicity have been reported during concomitant administration of lithium with angiotensin converting enzyme inhibitors and angiotensin II antagonists. Therefore, use of olmesartan medoxomil and lithium in combination is not recommended. If use of the combination proves necessary, careful monitoring of serum lithium levels is recommended.
Other compounds:
Compounds which have been investigated in specific clinical studies in healthy volunteers include warfarin, digoxin, an antacid (magnesium aluminium hydroxide), hydrochlorothiazide and pravastatin. No clinically relevant interactions were observed and in particular olmesartan medoxomil had no significant effect on the pharmacokinetics or pharmacodynamics of warfarin or the pharmacokinetics of digoxin.
Olmesartan had no clinically relevant inhibitory effects on in vitro human cytochrome P450 enzymes 1A1/2, 2A6, 2C8/9, 2C19, 2D6, 2E1 and 3A4, and had no or minimal inducing effects on rat cytochrome P450 activities. Therefore, in vivo interaction studies with known cytochrome P450 enzyme inhibitors and inducers were not conducted, and no clinically relevant interactions between olmesartan and drugs metabolised by the above cytochrome P450 enzymes are expected.
Chlorthalidone
Chlorthalidone may add to or potentiate the action of other antihypertensive drugs. Chlorthalidone and related drugs may increase the responsiveness to tubocurarine. Lithium renal clearance is reduced by chlorthalidone, increasing the risk of lithium toxicity. Monitor serum lithium levels during concomitant use.
4.6 Use in special populations
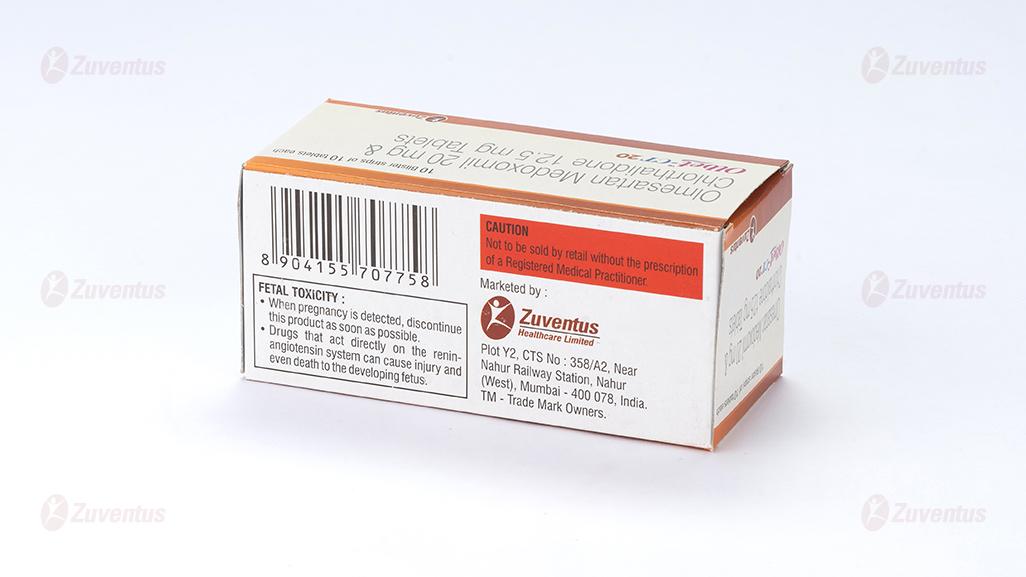
Pregnancy
Use of Olbet CT is Not recommended in pregnancy.
Breast-feeding
Use of Olbet CT is Not recommended in breast-feeding.
4.7 Effects on ability to drive and use machines
Olmesartan medoxomil has minor or moderate influence on the ablility to drive and use machines. Dizziness or fatigue may occasionally occur in patients taking antihypertensive therapy, which may impair the ablility to react.
4.8 Undesirable effects
Olmesartan medoxomil
The most commonly reported adverse reactions during treatment with olmesartan are headache (7.7%), influenza-like symptoms (4.0%) and dizziness (3.7%).
In placebo-controlled monotherapy studies, the only adverse drug reaction that was unequivocally related to treatment was dizziness (2.5% incidence on olmesartan medoxomil and 0.9% on placebo).
The incidence was also somewhat higher on olmesartan medoxomil compared with placebo for hypertriglyceridaemia (2.0% versus 1.1%) and for raised creatine phosphokinase (1.3% versus 0.7%).
The following terminologies have been used in order to classify the occurrence of adverse reactions very common (≥1/10); common (≥1/100 to <1/10); uncommon (≥1/1,000 to <1/100); rare (≥1/10,000 to <1/1,000); very rare (<1/10,000).
- Blood and lymphatic system disorders: Thrombocytopenia (Uncommon)
- Immune system disorders: Anaphylactic reaction (Uncommon)
- Metabolism and nutrition disorders: Hypertriglyceridaemia, Hyperuricaemia (Common), Hyperkalaemia (Rare)
- Nervous system disorders: Dizziness, Headache (Common)
- Ear and labyrinth disorders: Vertigo (Uncommon)
- Cardiac disorders: Angina pectoris (Uncommon)
- Vascular disorders: Hypotension (Rare)
- Respiratory, thoracic and mediastinal disorders: Bronchitis, Pharyngitis, Cough, Rhinitis (Common)
- Gastrointestinal disorders: Gastroenteritis, Diarrhoea, Abdominal pain, Nausea, Dyspepsia (Common), Vomiting (Uncommon), Sprue-like enteropathy (Very rare)
- Skin and subcutaneous tissue disorders: Exanthema, Allergic dermatitis, Urticaria, Rash, Pruritus, (Uncommon), Angioedema (Rare)
- Musculoskeletal and connective tissue disorders: Arthritis, Back pain, Skeletal pain, Myalgia, (Uncommon), Muscle spasm (Rare)
- Renal and urinary disorders: Haematuria, Urinary tract infection (common), Acute renal failure, Renal insufficiency (Rare)
- General disorders and administration site conditions: Pain, Chest pain, Peripheral oedema, Influenza-like symptoms, Fatigue (Common), Face oedema, Asthenia, Malaise (Uncommon), Lethargy (Rare)
- Investigations: Hepatic enzymes increased, Blood urea increased, Blood creatine phosphokinase increased (Common), Blood creatinine increased (Rare)
Chlorthalidone
- Hypotension
- Impaired Renal Function
- Electrolyte Abnormalities
- Metabolic Disturbances (see Warnings and Precautions for more information)
The following adverse reactions have been observed, but there is not enough systematic collection of data to support an estimate of their frequency.
Gastrointestinal System Reactions: anorexia, gastric irritation, nausea, vomiting, cramping, diarrhea, constipation, jaundice (intrahepatic cholestatic jaundice), pancreatitis.
Central Nervous System Reactions: dizziness, paresthesias, headache.
Hematologic Reactions: leukopenia, agranulocytosis, thrombocytopenia, aplastic anemia.
Dermatologic-Hypersensitivity Reactions: purpura, photosensitivity, rash, urticaria, necrotizing angiitis (vasculitis) (cutaneous vasculitis), Lyell’s syndrome (toxic epidermal necrolysis).
Cardiovascular Reaction: Orthostatic hypotension.
Other Adverse Reactions: muscle spasm, weakness, restlessness, impotence, xanthopsia.
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via email to: medico@zuventus.com
4.9 Overdose
Olmesartan medoxomil
Only limited information is available regarding overdosage in humans. The most likely effect of overdosage is hypotension. In the event of overdosage, the patient should be carefully monitored and treatment should be symptomatic and supportive.
No information is available regarding the dialysability of olmesartan.
Chlorthalidone
Symptoms of acute overdosage include nausea, weakness, dizziness and disturbances of electrolyte balance. The oral LD50 of the drug in the mouse and the rat is more than 25,000 mg/kg body weight. The minimum lethal dose (MLD) in humans has not been established. There is no specific antidote but gastric lavage is recommended, followed by supportive treatment. Where necessary, this may include intravenous dextrose-saline with potassium, administered with caution.
5.0 Pharmacological properties
5.1 Mechanism of Action
Olmesartan medoxomil
Olmesartan medoxomil is a potent, orally active, selective angiotensin II receptor (type AT1) antagonist. It is expected to block all actions of angiotensin II mediated by the AT1 receptor, regardless of the source or route of synthesis of angiotensin II.
Angiotensin II is the primary vasoactive hormone of the renin-angiotensin-aldosterone system and plays a significant role in the pathophysiology of hypertension via the type 1 (AT1) receptor.
Chlorthalidone
Chlorthalidone is a long-acting oral diuretic with antihypertensive activity. The diuretic effects of chlorthalidone and the benzothiadiazine (thiazide) diuretics appear to arise from similar mechanisms and the maximal effect of chlorthalidone and the thiazides appear to be similar. The site of the action appears to be the distal convoluted tubule of the nephron. Although the mechanism of action of chlorthalidone and related drugs is not wholly clear, sodium and water depletion appear to provide a basis for its antihypertensive effect.
5.2 Pharmacodynamic properties
Olmesartan medoxomil
The selective antagonism of the angiotensin II (AT1) receptors results in increases in plasma renin levels and angiotensin I and II concentrations, and some decrease in plasma aldosterone concentrations.
Chlorthalidone
The diuretic action of chlorthalidone commences a mean of 2.6 hours after dosing and continues for up to 72 hours. The drug produces diuresis with increased excretion of sodium and chloride. The diuretic effects of chlorthalidone lead to decreased extracellular fluid volume, plasma volume, cardiac output, total exchangeable sodium, glomerular filtration rate, and renal plasma flow. Chlorthalidone produces dose-related reductions in serum potassium levels, elevations in serum uric acid and blood glucose, and it can lead to decreased sodium and chloride levels.
5.3 Pharmacokinetic properties
Absorption and distribution
Olmesartan medoxomil
Olmesartan medoxomil is a prodrug. It is rapidly converted to the pharmacologically active metabolite, olmesartan, by esterases in the gut mucosa and in portal blood during absorption from the gastrointestinal tract.
No intact olmesartan medoxomil or intact side chain medoxomil moiety have been detected in plasma or excreta. The mean absolute bioavailability of olmesartan from a tablet formulation was 25.6 %.
The mean peak plasma concentration (Cmax) of olmesartan is reached within about 2 hours after oral dosing with olmesartan medoxomil, and olmesartan plasma concentrations increase approximately linearly with increasing single oral doses up to about 80 mg.
Food had minimal effect on the bioavailability of olmesartan and therefore olmesartan medoxomil may be administered with or without food.
No clinically relevant gender-related differences in the pharmacokinetics of olmesartan have been observed. Olmesartan is highly bound to plasma protein (99.7 %), but the potential for clinically significant protein binding displacement interactions between olmesartan and other highly bound coadministered drugs is low (as confirmed by the lack of a clinically significant interaction between olmesartan medoxomil and warfarin). The binding of olmesartan to blood cells is negligible. The mean volume of distribution after intravenous dosing is low (16 - 29 L).
Chlorthalidone
Absorption of chlorthalidone following oral dosing is consistent but incomplete (approximately 60%) with peak plasma concentrations occurring about 12 hours after dosing. The chlorthalidone blood levels are consistent and subject to little variability. In the blood, approximately 75% of the drug is bound to plasma proteins over a concentration range of 0.2 to 7.7 ug/mL.
Biotransformation and elimination
Olmesartan medoxomil
Total plasma clearance was typically 1.3 L/h (CV, 19 %) and was relatively slow compared to hepatic blood flow (ca 90L/h). Following a single oral dose of 14C-labelled olmesartan medoxomil, 10 - 16 % of the administered radioactivity was excreted in the urine (the vast majority within 24 hours of dose administration) and the remainder of the recovered radioactivity was excreted in the faeces. Based on the systemic availability of 25.6 %, it can be calculated that absorbed olmesartan is cleared by both renal excretion (ca 40 %) and hepato-biliary excretion (ca 60 %). All recovered radioactivity was identified as olmesartan. No other significant metabolite was detected. Enterohepatic recycling of olmesartan is minimal. Since a large proportion of olmesartan is excreted via the biliary route, use in patients with biliary obstruction is contraindicated.
The terminal elimination half-life of olmesartan varied between 10 and 15 hours after multiple oral dosing. Steady state was reached after the first few doses and no further accumulation was evident after 14 days of repeated dosing. Renal clearance was approximately 0.5 - 0.7 L/h and was independent of dose.
Chlorthalidone
The mean plasma half-life of chlorthalidone is about 40 to 60 hours. It is eliminated primarily as unchanged drug in the urine.
6.0 Nonclinical properties
6.1 Animal Toxicology or Pharmacology
Olmesartan medoxomil
In chronic toxicity studies in rats and dogs, olmesartan medoxomil showed similar effects to other AT1 receptor antagonists and ACE inhibitors: raised blood urea (BUN) and creatinine (through functional changes to the kidneys caused by blocking AT1 receptors); reduction in heart weight; a reduction of red cell parameters (erythrocytes, haemoglobin, haematocrit); histological indications of renal damage (regenerative lesions of the renal epithelium, thickening of the basal membrane, dilatation of the tubules). These adverse effects caused by the pharmacological action of olmesartan medoxomil have also occurred in preclinical trials on other AT1 receptor antagonists and ACE inhibitors and can be reduced by simultaneous oral administration of sodium chloride.
In both species, increased plasma renin activity and hypertrophy/hyperplasia of the juxtaglomerular cells of the kidney were observed. These changes, which are a typical effect of the class of ACE inhibitors and other AT1 receptor antagonists, would appear to have no clinical relevance.
Like other AT1 receptor antagonists olmesartan medoxomil was found to increase the incidence of chromosome breaks in cell cultures in vitro. No relevant effects were observed in several in vivo studies using olmesartan medoxomil at very high oral doses of up to 2000 mg/kg. The overall data of a comprehensive genotoxicity testing suggest that olmesartan is very unlikely to exert genotoxic effects under conditions of clinical use.
Olmesartan medoxomil was not carcinogenic, neither in rats in a 2 year study nor in mice when tested in two 6 month carcinogenicity studies using transgenic models.
In reproductive studies in rats, olmesartan medoxomil did not affect fertility and there was no evidence of a teratogenic effect. In common with other angiotensin II antagonists, survival of offspring was reduced following exposure to olmesartan medoxomil and pelvic dilatation of the kidney was seen after exposure of the dams in late pregnancy and lactation. In common with other antihypertensive agents, olmesartan medoxomil was shown to be more toxic to pregnant rabbits than to pregnant rats, however, there was no indication of a fetotoxic effect.
Chlorthalidone
Reproduction studies have been performed in the rat and the rabbit at doses up to 420 times the human dose and have revealed no evidence of harm to the fetus due to chlorthalidone. There are, however, no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Carcinogenesis, Mutagenesis, Impairment of Fertility: No information is available.
7.0 Description
Olmesartan medoxomil, a prodrug, is hydrolyzed to olmesartan during absorption from the gastrointestinal tract. Olmesartan is a selective AT 1 subtype angiotensin II receptor antagonist. Olmesartan medoxomil, USP is described chemically as 2,3-dihydroxy-2-butenyl 4-(1-hydroxy-1-methylethyl)-2-propyl-1-[ p-(o-1 H-tetrazol-5-ylphenyl)benzyl]imidazole-5-carboxylate, cyclic 2,3-carbonate.
Chlorthalidone is an antihypertensive/diuretic supplied as 15 mg and 25 mg tablets for oral use. It is a monosulfamyl diuretic that differs chemically from thiazide diuretics in that a double ring system is incorporated in its structure. It is a racemic mixture of 2-chloro-5-(1-hydroxy-3-oxo-1-isoindolinyl) benzenesulfonamide
8.0 Pharmaceutical particulars
8.1 Incompatibilities
Not applicable.
8.2 Shelf-life
Refer on pack
8.3 Packaging information
10 blister strips of 10 tablets each
8.8 Storage and handing instructions
Store protected from light & moisture at a temperature not exceeding 30°C.
Keep out of reach of children.
Tablet should be swallowed whole & not to be broken, chewed or crushed.
9.0 Patient Counselling Information
- Advice patients not to take this medicine, if they are allergic to Olmesartan Medoxomil or Chlorthalidone
- Signs of an allergic reaction include a rash, itching or shortness of breath.
- Symptomatic hypotension and syncope: Advise patients that light headedness can occur, especially during the first days of therapy, and to report this symptom to a healthcare provider. Inform patients that dehydration from inadequate fluid intake, excessive perspiration, vomiting, or diarrhea may lead to an excessive fall in blood pressure. If syncope occurs advise patients, to contact their healthcare provider.
- Pregnancy: Tell female patients Olbet CT should not be given during pregnancy and lactation.
- Discuss treatment options with women planning to become pregnant. Tell patients to report pregnancies to their physicians as soon as possible.
- Tell the patients if they get any side effects, talk to the doctor or pharmacist. This includes any possible side effects not listed in this leaflet.
- Advice patients if they have any further questions, ask the doctor or pharmacist.
12.0 Date of revision
11/10/2024
About Leaflet
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor or pharmacist.
- This medicine has been prescribed for you. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet. See section 4.
What is in this leaflet
1. What OLBET CT is and what it is used for
2. What you need to know before you take OLBET CT
3. How to take OLBET CT
4. Possible side effects
5. How to store OLBET CT
6. Contents of the pack and other information
1. What Olbet Ct is and What It is Used for
OLBET CT tablets is a combination of Olmesartan Medoxomil and Chlorthalidone (20mg/12.5mg, 40mg/12.5mg).
Olmesartan and Chlorthalidone are used for the treatment of high blood pressure (also known as ‘hypertension’).
High blood pressure can damage blood vessels in organs such as the heart, kidneys, brain and eyes. In some cases, this may lead to a heart attack, heart or kidney failure, stroke or blindness. Usually high blood pressure has no symptoms. It is important to have your blood pressure checked to prevent damage occurring.
High blood pressure can be controlled with medicines such as OLBET CT Tablets. Your doctor has probably also recommended that you make some changes to your lifestyle to help lower your blood pressure (for example losing weight, giving up smoking, reducing the amount of alcohol you drink and reducing the amount of salt in your diet). Your doctor may also have urged you to take regular exercise, such as walking or swimming. It is important to follow this advice from your doctor.
2. What You Need to Know Before You Take Olbet Ct
Do not use OLBET CT
- If you are allergic to olmesartan medoxomil or chlorthalidone.
- If you are pregnant.
- If you suffer from yellowing of the skin and eyes (jaundice) or problems with drainage of the bile from the gallbladder (biliary obstruction e.g. Gallstones).
- If you have diabetes or impaired kidney function and you are treated with a blood pressure lowering medicine containing aliskiren. If you are not able to pass urine or passing an insignificant amount of urine
Warnings and precautions
Talk to your doctor, pharmacist or nurse before using OLBET CT
- Tell your doctor if you are taking any of the following medicines used to treat high blood pressure:
- An ACE-inhibitor (for example enalapril, lisinopril, ramipril), in particular if you have diabetes-related kidney problems.
- Aliskiren
- Your doctor may check your kidney function, blood pressure, and the amount of electrolytes (e.g. potassium) in your blood at regular intervals.
- See also information under the heading “Do not take OLBET CT Tablets”
Tell your doctor if you have any of the following health problems:
- Kidney problems
- Liver disease
- Heart failure or problems with your heart valves or heart muscle
- Severe vomiting, diarrhoea, treatment with high doses of water tablets (diuretics) or if you are on a low salt diet
- Increased levels of potassium in your blood
- Problems with your adrenal glands.
Contact your doctor if you experience diarrhoea that is severe, persistent and causes substantial weight loss. Your doctor may evaluate your symptoms and decide on how to continue your blood pressure medication.
As with any medicine which reduces blood pressure, an excessive drop in blood pressure in patients with blood flow disturbances of the heart or brain could lead to a heart attack or stroke. Your doctor will therefore check your blood pressure carefully.
You must tell your doctor if you think you are (or might become) pregnant. OLBET CT tablets are not recommended in pregnancy.
Other medicines and OLBET CT
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines. In particular, tell your doctor or pharmacist about any of the following:
- Other blood pressure lowering medicines, as the effect of OLBET CT Tablets can be increased. Your doctor may need to change your dose and/or to take other precautions: If you are taking an ACE-inhibitor or aliskiren (see also information under the headings “Do not take OLBET CT Tablets ” and “Warnings and precautions”)
- Potassium supplements, a salt substitute which contains potassium, water tablets (diuretics) or heparin (for thinning the blood). Using these medicines at the same time as OLBET CT Tablets may raise the levels of potassium in your blood.
- Lithium (a medicine used to treat mood swings and some types of depression) used at the same time as OLBET CT Tablets may increase the toxicity of lithium. If you have to take lithium, your doctor will measure your lithium blood levels
- Non-Steroidal Anti-Inflammatory (NSAIDs) medicines (medicines used to relieve pain, swelling and other symptoms of inflammation, including arthritis) used at the same time as OLBET CT Tablets may increase the risk of kidney failure and the effect of OLBET CT Tablets can be decreased by NSAIDs
- Colesevelam hydrochloride, a drug that lowers the level of cholesterol in your blood, as the effect of OLBET CT may be decreased. Your doctor may advise you to take OLBET CT at least 4 hours before colesevelam hydrochloride.
- Certain antacids (indigestion remedies), as the effect of OLBET CT Tablets can be slightly decreased.
- OLBET CT may increase the responsiveness to tubocurarine.
Pregnancy
You must tell your doctor if you think you are (or might become) pregnant. Your doctor will advise you to stop taking OLBET CT Tablets before you become pregnant or as soon as you know you are pregnant and will advise you to take another medicine instead of OLBET CT Tablets. OLBET CT Tablets are not recommended in pregnancy.
Breast-feeding
Tell your doctor if you are breast-feeding or about to start breast-feeding. OLBET CT Tablets are not recommended for mothers who are breast-feeding, and your doctor may choose another treatment for you.
Driving and using machines
You may feel sleepy or dizzy while being treated for your high blood pressure. If this happens, do not drive or use machines until the symptoms wear off. Ask your doctor for advice.
3. How to Take Olbet Ct
Always take this medicine exactly as your doctor has told you. Check with your doctor or pharmacist if you are not sure.
The dose of OLBET CT is one tablet once daily.
If your blood pressure is not controlled, your doctor may increase your dose from OLBET CT 20 to OLBET CT 40 once a day, or prescribe additional medicines.
Safety and effectiveness of Olbet CT in children have not been established.
Patients with kidney problems
In patients with mild to moderate kidney disease, your dose will not be higher than OLBET CT 20 once a day.
If you take more OLBET CT than you should
If you take more tablets than you should or if a child accidentally swallows some, go to your doctor or nearest emergency department immediately and take your medicine pack with you.
If you miss a dose of OLBET CT
If you forget a dose, take your normal dose on the following day as usual. Do not take a double dose to make up for a forgotten tablet.
If you stop taking OLBET CT Tablets
It is important to continue to take OLBET CT Tablets unless your doctor tells you to stop. If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
4. Possible Side Effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
If they do occur, they are often mild and do not require treatment to be stopped.
Although not many people may get them, the following two side effects can be serious:
Olmesartan medoxomil
On rare occasions (may affect up to 1 in 1,000 people) the following allergic reactions, that may affect the whole body have been reported: Swelling of the face, mouth and/or larynx (voice box) together with itching and rash may occur during treatment with Olmesartan. If this happens stop taking OLBET CT Tablets and contact your doctor immediately.
Rarely (but slightly more often in older people) Olmesartan can cause the blood pressure to fall too low in susceptible individuals or as the result of an allergic reaction. This could cause severe light-headedness or fainting. If this occurs stop taking OLBET CT Tablets, contact your doctor immediately and lie down flat.
These are the other side effects known about so far with Olmesartan:
Common side effects (may affect up to 1 in 10 people): Dizziness, headache, nausea, indigestion, diarrhoea, stomach ache, gastroenteritis, tiredness, sore throat, runny or stuffy nose, bronchitis, flu-like symptoms, cough, pain, pain in the chest, back, bones or joints, infection of the urinary tract, swelling of ankles, feet, legs, hands or arms, blood in the urine.
Some changes in blood test results have also been seen and include the following: Increased fat levels (hypertriglyceridaemia), increased uric acid levels (hyperuricaemia), rise in blood urea, increases in tests of liver and muscle function.
Uncommon side effects (may affect up to 1 in 100 people): Quick allergic reactions that may affect the whole body and may cause breathing problems as well as a rapid fall of blood pressure that may even lead to fainting (anaphylactic reactions), swelling of the face, vertigo, vomiting, weakness, feeling unwell, muscular pain, skin rash, allergic skin rash, itching, exanthema (skin eruption), skin lumps (wheals), angina (pain or uncomfortable feeling in the chest). In blood tests a reduction of the numbers of a type of blood cell, known as platelets has been seen (thrombocytopenia).
Rare side effects (may affect up to 1 in 1,000 people): Lack of energy, muscle cramps, impaired kidney function, kidney failure.
Some changes in blood test results have also been seen. These include increased potassium levels (hyperkalaemia) and increased levels of compounds related to kidney function.
Chlorthalidone
The following adverse reactions have been observed, but there is not enough systematic collection of data to support an estimate of their frequency.
Gastrointestinal System Reactions: anorexia, gastric irritation, nausea, vomiting, cramping, diarrhea, constipation, jaundice (intrahepatic cholestatic jaundice), pancreatitis.
Central Nervous System Reactions: dizziness, paresthesias, headache. Hematologic Reactions: leukopenia, agranulocytosis, thrombocytopenia, aplastic anemia.
Dermatologic-Hypersensitivity Reactions: purpura, photosensitivity, rash, urticaria, necrotizing angiitis (vasculitis) (cutaneous vasculitis), Lyell’s syndrome (toxic epidermal necrolysis).
Cardiovascular Reaction: Orthostatic hypotension.
Other Adverse Reactions: muscle spasm, weakness, restlessness, impotence, xanthopsia.
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly: Website: www.zuventus.co.in and click the tab “Safety Reporting” located on the top right end of the home page.
By reporting side effects, you can help provide more information on the safety of this medicine.
You can also report the side effect with the help of your treating physician.
5. How to Store Olbet Ct
Store protected from light & moisture at a temperature not exceeding 30°C.
Keep out of reach of children.
Tablet should be swallowed whole & not to be broken, chewed or crushed.
6. Contents of the Pack and Other Information
What OLBET CT contains
OLBET CT contains combination of Olmesartan Medoxomil and Chlorthalidone. (20mg/12.5mg, 40mg/12.5mg).
Olbet-CT 20 Tablets
Each film coated bilayered tablets contains:
Olmesartan Medoxomil IP ………. 20mg
Chlorthalidone IP …………………………..12.5 mg
Excipients……………………………………..q.s.
Olbet-CT 40 Tablets
Each film coated bilayered tablets contains:
Olmesartan Medoxomil IP ………. 40mg
Chlorthalidone IP ………………………..12.5 mg
Excipients……………………………………..q.s.