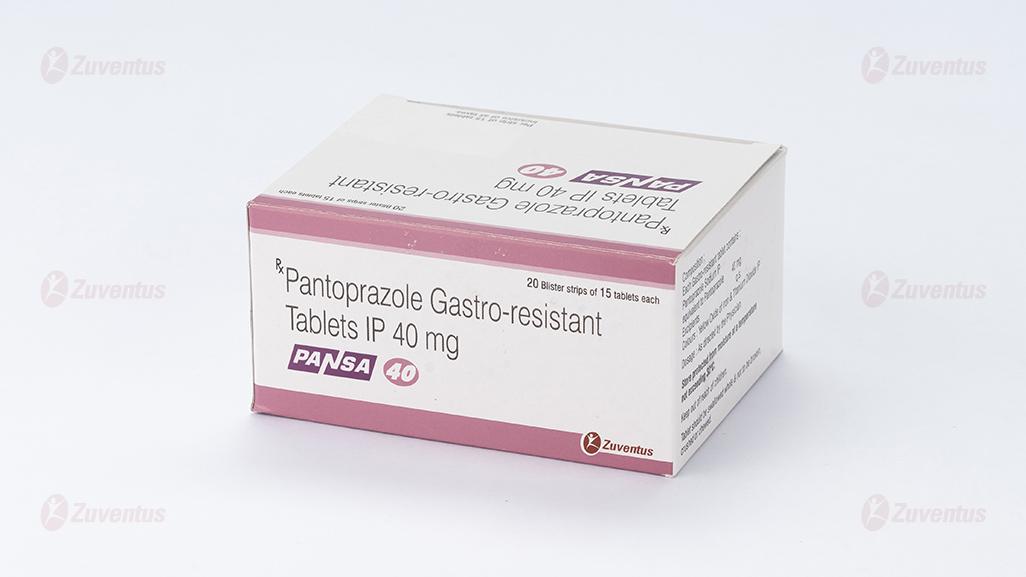
Pansa 40 Tablets
Therapy Area
Gastrointestinal
1.0 Generic name
Pantoprazole Gastro-resistant Tablets IP 40 mg
2.0 Qualitative and quantitative composition
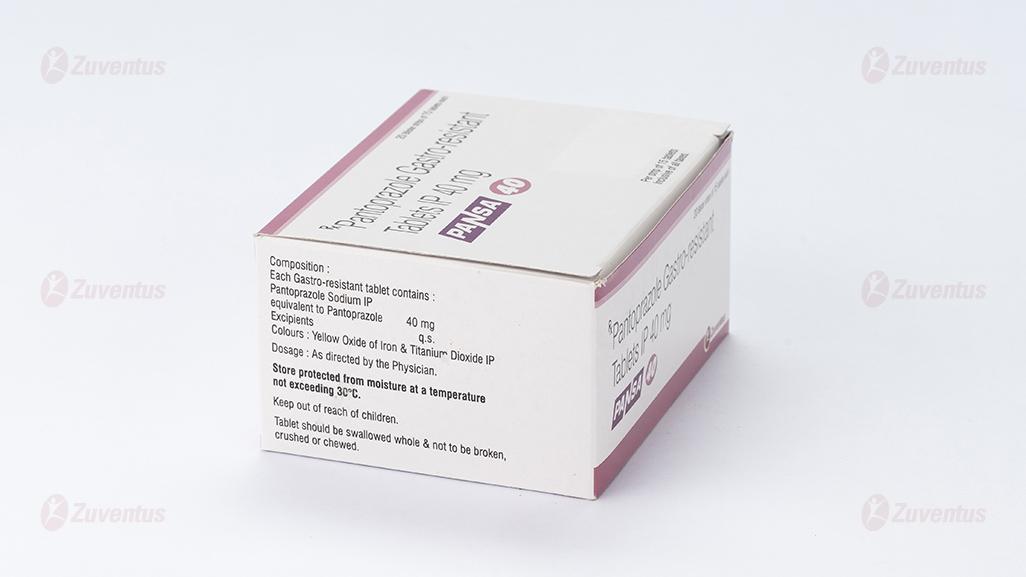
Each Gastro-resistant tablet contains :
Pantoprazole Sodium IP
equivalent to Pantoprazole 40 mg
Excipients q.s.
Colours : Yellow Oxide of Iron &
Titanium Dioxide IP
3.0 Dosage form and strength
Gastro-resistant Tablet 40 mg
4.0 Clinical particulars
4.1 Therapeutic indication
For the treatment of gastric ulcer, duodenal ulcer, moderate and severe reflux oesophagitis.
4.2 Posology and method of administration Adults and adolescents 12 years of age and above Reflux oesophagitis
One tablet of Pantoprazole per day. In individual cases the dose may be doubled (increase to 2 tablets Pantoprazole daily) especially when there has been no response to other treatment. A 4-week period is usually required for the treatment of reflux oesophagitis. If this is not sufficient, healing will usually be achieved within a further 4 weeks.
Treatment of gastric ulcer
One tablet of Pantoprazole per day. In individual cases the dose may be doubled (increase to 2 tablets of Pantoprazole daily) especially when there has been no response to other treatment. A 4-week period is usually required for the treatment of gastric ulcers. If this is not sufficient, healing will usually be achieved within a further 4 weeks.
Treatment of duodenal ulcer
One tablet of Pantoprazole per day. In individual cases the dose may be doubled (increase to 2 tablets of Pantoprazole daily) especially when there has been no response to other treatment. A duodenal ulcer generally heals within 2 weeks. If a 2-week period of treatment is not sufficient, healing will be achieved in almost all cases within a further 2 weeks.
Special populations
Patients with hepatic impairment
A daily dose of 20 mg Pantoprazole (1 tablet of 20 mg Pantoprazole) should not be exceeded in patients with severe liver impairment.
Patients with renal impairment
No dose adjustment is necessary in patients with impaired renal function
Elderly
No dose adjustment is necessary in the elderly
Paediatric population
Pantoprazole is not recommended for use in children below 12 years of age because of limited data on safety and efficacy in this age group.
Method of administration
Oral use. The tablets should not be chewed or crushed, and should be swallowed whole 1 hour before a meal with some water
4.3 Contraindications
Hypersensitivity to the active substance, substituted Benzimidazoles, or to any of the excipients listed in the formulation
4.4 Warning and precautions
Hepatic impairment
In patients with severe liver impairment, the liver enzymes should be monitored regularly during treatment with Pantoprazole, particularly on long-term use. In the case of a rise of the liver enzymes, the treatment should be discontinued.
Gastric malignancy
Symptomatic response to Pantoprazole may mask the symptoms of gastric malignancy and may delay diagnosis. In the presence of any alarm symptom (e.g. significant unintentional weight loss, recurrent vomiting, dysphagia, haematemesis, anaemia or melaena) and when gastric ulcer is suspected or present, malignancy should be excluded. Further investigation is to be considered if symptoms persist despite adequate treatment.
Co-administration with HIV protease inhibitors
Co-administration of Pantoprazole is not recommended with HIV protease inhibitors for which absorption is dependent on acidic intragastric pH such as Atazanavir, due to significant reduction in their bioavailability.
Long-term treatment
In long-term treatment, especially when exceeding a treatment period of 1 year, patients should be kept under regular surveillance
Gastrointestinal infections caused by bacteria
Treatment with Pantoprazole may lead to a slightly increased risk of gastrointestinal infections caused by bacteria such as Salmonella and Campylobacter or C. difficile.
Hypomagnesaemia
Severe hypomagnesaemia has been rarely reported in patients treated with proton pump inhibitors (PPIs) like Pantoprazole for at least three months, and in most cases for a year. Serious manifestations of hypomagnesaemia such as fatigue, tetany, delirium, convulsions, dizziness and ventricular arrhythmia can occur but they may begin insidiously and be overlooked. Hypomagnesaemia may lead to hypocalcaemia and/or hypokalaemia. In most affected patients, hypomagnesaemia (and hypomagnesaemia associated hypocalcaemia and/or hypokalaemia) improved after magnesium replacement and discontinuation of the PPI.
For patients expected to be on prolonged treatment or who take PPIs with digoxin or medicinal products that may cause hypomagnesaemia (e.g. diuretics), health care professionals should consider measuring magnesium levels before starting PPI treatment and periodically during treatment.
Bone fractures
Proton pump inhibitors, especially if used in high doses and over long durations (> 1 year), may modestly increase the risk of hip, wrist and spine fracture, predominantly in the elderly or in the presence of other recognised risk factors. Observational studies suggest that proton pump inhibitors may increase the overall risk of fracture by 10 - 40%. Some of this increase may be due to other risk factors. Patients at risk of osteoporosis should receive care according to current clinical guidelines and they should have an adequate intake of vitamin D and calcium
Sub-acute cutaneous lupus erythematosus (SCLE)
Proton pump inhibitors are associated with very infrequent cases of SCLE. If lesions occur, especially in sun exposed areas of the skin, and if accompanied by arthralgia, the patient should seek medical help promptly and the healthcare professional should consider stopping Pantoprazole. SCLE after previous treatment with a proton pump inhibitor may increase the risk of SCLE with other proton pump inhibitors.
Interference with laboratory tests
Increased Chromogranin A (CgA) level may interfere with investigations for neuroendocrine tumours. To avoid this interference, Pantoprazole treatment should be stopped for at least 5 days before CgA measurements. If CgA and gastrin
levels have not returned to reference range after initial measurement, measurements should be repeated 14 days after cessation of proton pump inhibitor treatment.
4.5 Drug interactions
Medicinal products with pH-dependent absorption pharmacokinetics
Because of profound and long-lasting inhibition of gastric acid secretion, Pantoprazole may interfere with the absorption of medicinal products where gastric pH is an important determinant of oral bioavailability, e.g. some azole antifungals such as Ketoconazole, Itraconazole, Posaconazole and other medicines such as Erlotinib.
HIV protease inhibitors
Co-administration of Pantoprazole is not recommended with HIV protease inhibitors for which absorption is dependent on acidic intragastric pH such as Atazanavir due to significant reduction in their bioavailability. If the combination of HIV protease inhibitors with a proton pump inhibitor is judged unavoidable, close clinical monitoring (e.g. virus load) is recommended. A Pantoprazole dose of 20 mg per day should not be exceeded. Dosage of the HIV protease inhibitor may need to be adjusted.
Coumarin anticoagulants (Phenprocoumon or Warfarin)
Co-administration of Pantoprazole with Warfarin or Phenprocoumon did not affect the pharmacokinetics of Warfarin, Phenprocoumon or INR. However, there have been reports of increased INR and prothrombin time in patients receiving PPIs and Warfarin or Phenprocoumon concomitantly. Increases in INR and prothrombin time may lead to abnormal bleeding, and even death. Patients treated with Pantoprazole and Warfarin or Phenprocoumon may need to be monitored for increase in INR and prothrombin time.
Methotrexate
Concomitant use of high-dose Methotrexate (e.g. 300 mg) and proton pump inhibitors has been reported to increase Methotrexate levels in some patients. Therefore, in settings where high-dose Methotrexate is used, for example cancer and psoriasis, a temporary withdrawal of Pantoprazole may need to be considered.
Other interactions studies
Pantoprazole is extensively metabolised in the liver via the cytochrome P450 enzyme system. The main metabolic pathway is demethylation by CYP2C19 and other metabolic pathways include oxidation by CYP3A4. Interaction studies with medicinal products also metabolised with these pathways, like Carbamazepine, Diazepam, Glibenclamide, Nifedipine, and an oral contraceptive containing Levonorgestrel and Ethinyl Oestradiol, did not reveal clinically significant interactions
An interaction of Pantoprazole with other medicinal products or compounds, which are metabolised using the same enzyme system, cannot be excluded.
Results from a range of interaction studies demonstrate that Pantoprazole does not affect the metabolism of active substances metabolised by CYP1A2 (such as Caffeine, Theophylline), CYP2C9 (such as Piroxicam, Diclofenac, Naproxen), CYP2D6 (such as Metoprolol), CYP2E1 (such as Ethanol), or does not interfere with p-glycoprotein related absorption of Digoxin.
There were no interactions with concomitantly administered antacids. Interaction studies have also been performed by concomitantly administering Pantoprazole with the respective antibiotics (Clarithromycin, Metronidazole, Amoxicillin). No clinically relevant interactions were found.
Medicinal products that inhibit or induce CYP2C19
Inhibitors of CYP2C19 such as fluvoxamine could increase the systemic exposure of Pantoprazole. A dose reduction may be considered for patients treated long-term with high doses of Pantoprazole, or those with hepatic impairment. Enzyme inducers affecting CYP2C19 and CYP3A4 such as Rifampicin and St John´s wort (Hypericum perforatum) may reduce the plasma concentrations of PPIs that are metabolised through these enzyme systems.
4.6 Special populations
Pregnancy
A moderate amount of data on pregnant women (between 300-1000 pregnancy outcomes) indicate no malformative or fetal/ neonatal toxicity of Pantoprazole. Animal studies have shown reproductive toxicity. As a precautionary measure, it is preferable to avoid the use of Pantoprazole during pregnancy.
Breast-feeding
Animal studies have shown excretion of Pantoprazole in breast milk. There is insufficient information on the excretion of Pantoprazole in human milk but excretion into human milk has been reported. A risk to the new-borns / infants cannot be excluded. Therefore, a decision on whether to discontinue breast-feeding or to discontinue/abstain from Pantoprazole therapy taking into account the benefit of breast-feeding for the child, and the benefit of Pantoprazole therapy for the woman.
Fertility
There was no evidence of impaired fertility following the administration of Pantoprazole in animal studies
4.7 Effects on ability to drive and use machines
Pantoprazole has no or negligible influence on the ability to drive and use machines. Adverse drug reactions, such as dizziness and visual disturbances may occur. If affected, patients should not drive or operate machines.
4.8 Undesirable effects
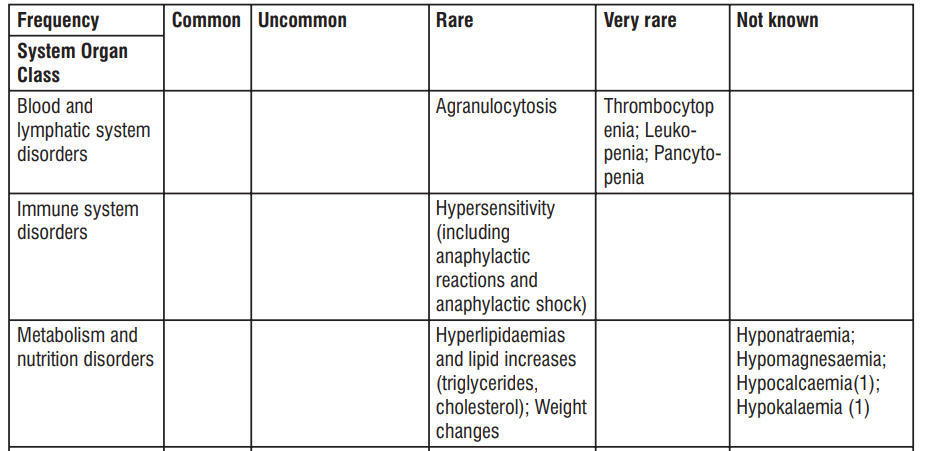
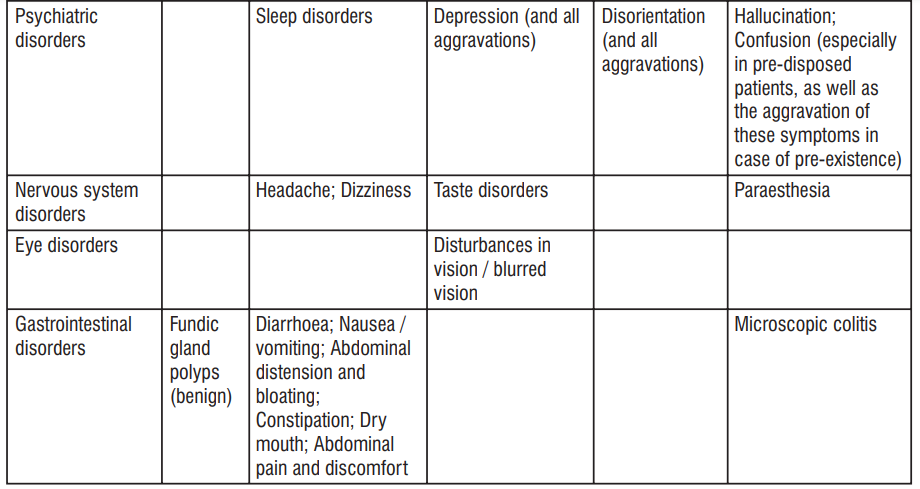
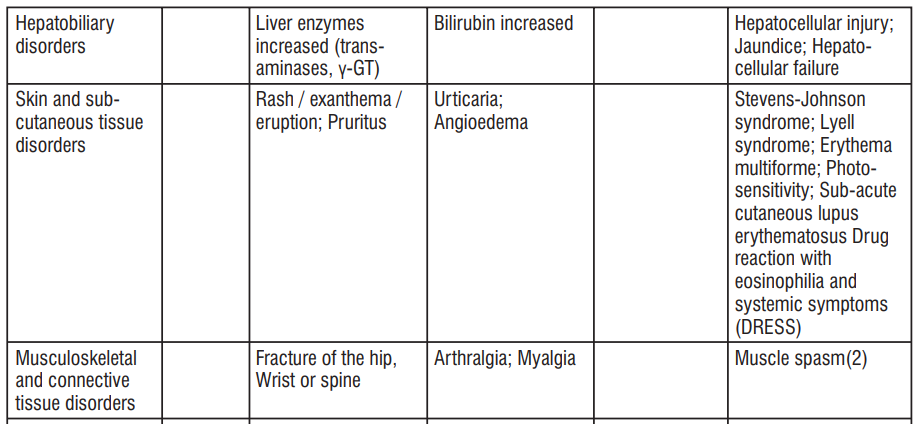
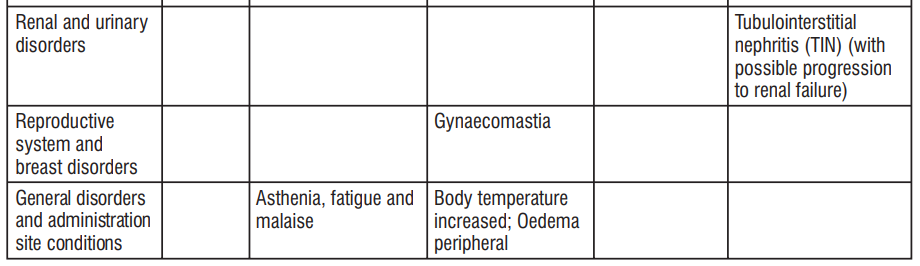
1. Hypocalcemia and/or hypokalaemia may be related to the occurrence of hypomagnesaemia in association with hypomagnesemia.
2. Muscle spasm as a consequence of electrolyte disturbance.
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via email to : medico@zuventus.com
By reporting side effects, you can help provide more information on the safety of this medicine.
4.9 Overdose
There are no known symptoms of overdose in man. Systemic exposure with up to 240 mg administered intravenously over 2 minutes, were well tolerated. As Pantoprazole is extensively protein bound, it is not readily dialysable. In the case of an overdose with clinical signs of intoxication, apart from symptomatic and supportive treatment, no specific therapeutic recommendations can be made.
5.0 Pharmacological properties
5.1 Mechanism of action
Pantoprazole is a substituted Benzimidazole which inhibits the secretion of Hydrochloric acid in the stomach by specific blockade of the proton pumps of the parietal cells. Pantoprazole is converted to its active form in the acidic environment in the parietal cells where it inhibits the H+, K+-ATPase enzyme, i.e. the final stage in the production of hydrochloric acid in the stomach. The inhibition is dose-dependent and affects both basal and stimulated acid secretion. In most patients, freedom from symptoms is achieved within 2 weeks. As with other proton pump inhibitors and H2 receptor inhibitors, treatment with Pantoprazole reduces acidity in the stomach and thereby increases gastrin in proportion to the reduction in acidity. The increase in gastrin is reversible. Since Pantoprazole binds to the enzyme distal to the cell receptor level, it can inhibit hydrochloric acid secretion independently of stimulation by other substances (Acetylcholine, Histamine, Gastrin). The effect is the same whether the product is given orally or intravenously.
5.2 Pharmacodynamic properties
The fasting gastrin values increase under Pantoprazole. On short-term use, in most cases they do not exceed the upper limit of normal. During long-term treatment, gastrin levels double in most cases. An excessive increase, however, occurs only in isolated cases. As a result, a mild to moderate increase in the number of specific endocrine (ECL) cells in the stomach is observed in a minority of cases during long-term treatment (simple to adenomatoid hyperplasia). However, according to the studies conducted so far, the formation of carcinoid precursors (atypical hyperplasia) or gastric carcinoids as were found in animal experiments have not been observed in humans. An influence of a long term treatment with Pantoprazole exceeding one year cannot be completely ruled out on endocrine parameters of the thyroid according to results in animal studies. During treatment with antisecretory medicinal products, serum gastrin increases in response to the decreased acid secretion. Also CgA increases due to decreased gastric acidity. The increased CgA level may interfere with investigations for neuroendocrine tumours. Available published evidence suggests that proton pump inhibitors should be discontinued between 5 days and 2 weeks prior to CgA measurements. This is to allow CgA levels that might be spuriously elevated following PPI treatment to return to reference range.
5.3 Pharmacokinetic properties
Absorption
Pantoprazole is rapidly absorbed and the maximal plasma concentration is achieved even after one single 40 mg oral dose. On average at about 2.5 h p.a. the maximum serum concentrations of about 2 - 3 µg/mL are achieved, and these values remain constant after multiple administration. Pharmacokinetics does not vary after single or repeated administration. In the dose range of 10 to 80 mg, the plasma kinetics of Pantoprazole are linear after both oral and intravenous administration. The absolute bioavailability from the tablet was found to be about 77%. Concomitant intake of food had no influence on AUC, maximum serum concentration and thus bioavailability. Only the variability of the lag-time will be increased by concomitant food intake.
Distribution
Pantoprazole's serum protein binding is about 98%. Volume of distribution is about 0.15 L/kg.
Biotransformation
The substance is almost exclusively metabolised in the liver. The main metabolic pathway is demethylation by CYP2C19 with subsequent sulphate conjugation; other metabolic pathway includes oxidation by CYP3A4.
Elimination
Terminal half-life is about 1 hour and clearance is about 0.1 L/h/kg. There were a few cases of subjects with delayed elimination. Because of the specific binding of Pantoprazole to the proton pumps of the parietal cell the elimination half-life does not correlate with the much longer duration of action (inhibition of acid secretion). Renal elimination represents the major route of excretion (about 80%) for the metabolites of Pantoprazole, the rest is excreted with the faeces. The main metabolite in both the serum and urine is desmethylpantoprazole which is conjugated with sulphate. The half-life of the main metabolite (about 1.5 hours) is not much longer than that of Pantoprazole.
6.0 Nonclinical properties
6.1 Animal toxicology or pharmacology
Non-clinical data reveal no special hazard to humans based on conventional studies of safety pharmacology, repeated dose toxicity and genotoxicity. In the two-year carcinogenicity studies in rats neuroendocrine neoplasms were found. In addition, squamous cell papillomas were found in the fore stomach of rats. The mechanism leading to the formation of gastric carcinoids by substituted Benzimidazoles has been carefully investigated and allows the conclusion that it is a secondary reaction to the massively elevated serum gastrin levels occurring in the rat during chronic high-dose treatment. In the two-year rodent
studies an increased number of liver tumours was observed in rats and in female mice and was interpreted as being due to Pantoprazole's high metabolic rate in the liver. A slight increase of neoplastic changes of the thyroid was observed in the group of rats receiving the highest dose (200 mg/kg). The occurrence of these neoplasms is associated with the pantoprazole-induced changes in the breakdown of thyroxine in the rat liver. As the therapeutic dose in man is low, no harmful effects on the thyroid glands are expected. In a peri-postnatal rat reproduction study designed to assess bone development, signs of offspring toxicity (mortality, lower mean body weight, lower mean body weight gain and reduced bone growth) were observed at exposures (Cmax) approximately 2x the human clinical exposure. By the end of the recovery phase, bone parameters were similar across groups and body weights were also trending toward reversibility after a drug-free recovery period. The increased mortality has only been reported in pre-weaning rat pups (up to 21 days age) which is estimated to correspond to infants up to the age of 2 years old. The relevance of this finding to the paediatric population is unclear. A previous peri-postnatal study in rats at slightly lower doses found no adverse effects at 3 mg/kg compared with a low dose of 5 mg/kg in this study. Investigations revealed no evidence of impaired fertility or teratogenic effects. Penetration of the placenta was investigated in the rat and was found to increase with advanced gestation. As a result, concentration of Pantoprazole in the foetus is increased shortly before birth.
7.0 Description
Pantoprazole is a proton pump inhibitor (PPI) that suppresses the final step in gastric acid production by covalently binding to the (H+, K+)-ATPase enzyme system at the secretory surface of the gastric parietal cell. It is a substituted benzimidazole, a compound that inhibits gastric acid secretion. Its chemical name is sodium 5-(difluoromethoxy)-2-[[(3,4-dimethoxy2-pyridinyOmethyl] sulfinyl] 1H-benzimidazole sesquihydrate. Its empirical formula is C16H14F2N3NaO4S. 1.5 H2O, with a molecular weight of 432.4 g/mol.
8.0 Pharmaceutical particulars
8.1 Incompatibilities
Not applicable
8.2 Shelf-life
Refer on the pack.
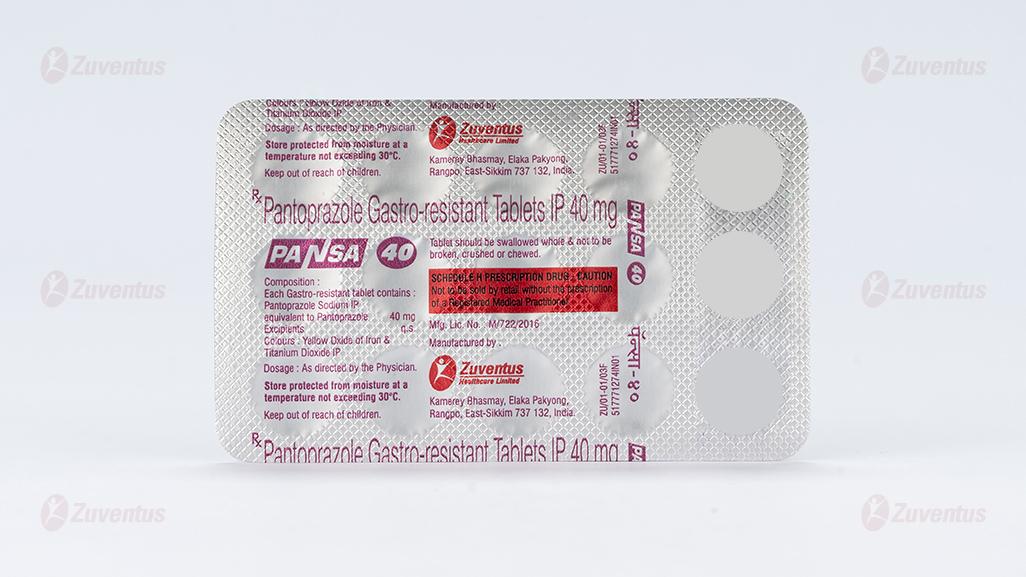
8.3 Packaging information
PVC/PVDC-Alu blister strip of 15 tablets.
8.4 Storage and handing instructions
Store protected from moisture at a temperature not exceeding 30°C.
Keep out of reach of children.
9.0 Patient counselling information
Do not take Pantoprazole
If you are allergic to Pantoprazole or to any of the other ingredients of this medicine.
If you are allergic to medicines containing other proton pump inhibitors.
Warnings and precautions
Talk to your doctor, pharmacist or nurse before taking Pantoprazole.
• If you have severe liver problems. Please tell your doctor if you have ever had problems with your liver in the past. Your doctor will check your liver enzymes more frequently, especially when you are taking Pantoprazole as a long-term treatment. In the case of a rise of liver enzymes the treatment should be stopped.
• If you have reduced body stores or risk factors for reduced Vitamin B12 and receive long-term treatment with Pantoprazole. As with all acid reducing agents, pantoprazole may lead to a reduced absorption of Vitamin B12.
• If you are taking HIV protease inhibitors such as Atazanavir (for the treatment of HIV-infection) at the same time as Pantoprazole, ask your doctor for specific advice.
• Taking a proton pump inhibitor like Pantoprazole, especially over a period of more than one year, may slightly increase your risk of fracture in the hip, wrist or spine. Tell your doctor if you have osteoporosis (reduced bone density) or if you have been told that you are at risk of getting osteoporosis (for example, if you are taking steroids).
• If you are on Pantoprazole for more than three months it is possible that the levels of Magnesium in your blood may fall. Low levels of magnesium can be seen as fatigue, involuntary muscle contractions, disorientation, convulsions, dizziness, increased heart rate. If you get any of these symptoms, please tell your doctor promptly. Low levels of magnesium can also lead to a reduction in Potassium or Calcium levels in the blood. Your doctor may decide to perform regular blood tests to monitor your levels of Magnesium.
• If you have ever had a skin reaction after treatment with a medicine similar to Pantoprazole that reduces stomach acid.
• If you get a rash on your skin, especially in areas exposed to the sun tell your doctor as soon as you can, as you may need to stop your treatment with Pantoprazole. Remember to also mention any other ill-effects like pain in your joints.
• If you are due to have a specific blood test (Chromogranin A).
Tell your doctor immediately, before or after taking this medicine, if you notice any of the following symptoms, which could be a sign of another, more serious, disease :
• An unintentional loss of weight.
• Vomiting, particularly if repeated.
• Vomiting blood; this may appear as dark coffee grounds in your vomit.
• You notice blood in your stools; which may be black or tarry in appearance.
• Difficulty in swallowing or pain when swallowing.
• You look pale and feel weak (anaemia)
• Chest pain
• Stomach pain
• Severe and/or persistent diarrhoea, because this medicine has been associated with a small increase in infectious diarrhoea
Your doctor may decide that you need some tests to rule out malignant disease because Pantoprazole also alleviates the symptoms of cancer and could cause delay in diagnosing it. If your symptoms continue in spite of your treatment, further investigations will be considered. If you take Pantoprazole on a long-term basis (longer than 1 year) your doctor will probably keep you under regular surveillance. You should report any new and exceptional symptoms and circumstances whenever you see your doctor.
Children and adolescents
Pantoprazole is not recommended for use in children as it has not been proven to work in children below 12 years of age.
Other medicines and Pantoprazole
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines, including medicines obtained without a prescription.
This is because Pantoprazole may influence the effectiveness of other medicines, so tell your doctor if you are taking :
• Medicines such as Ketoconazole, Itraconazole and Posaconazole (used to treat fungal infections) or Erlotinib (used for certain types of cancer) because Pantoprazole may stop these and other medicines from working properly.
• Warfarin and Phenprocoumon, which affect the thickening, or thinning of the blood. You may need further checks.
• Medicines used to treat HIV-infection, such as Atazanavir.
• Methotrexate (used to treat rheumatoid arthritis, psoriasis, and cancer) - if you are taking Methotrexate your doctor may temporarily stop your Pantoprazole treatment because Pantoprazole can increase levels of Methotrexate in the blood.
• Fluvoxamine (used to treat depression and other psychiatric diseases) if you are taking Fluvoxamine your doctor may reduce the dose.
• Rifampicin (used to treat infections).
• St John’s wort (Hypericum perforatum) (used to treat mild depression).
About leaflet
Read all of this leaflet carefully before you start taking this medicine because it contains important information for you.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor. This includes any possible side effects not listed in this leaflet. See section 4.
What is in this leaflet
1. What PANSA 40 is and what it is used for
2. What you need to know before you take PANSA 40
3. How to take PANSA 40
4. Possible side effects
5. How to store PANSA 40
6. Contents of the pack and other information
1. What PANSA 40 is and what it is used for
Pantoprazole contains the active substance pantoprazole. Pantoprazole is a selective “proton pump inhibitor”, a medicine which reduces the amount of acid produced in your stomach. It is used for treating acid-related diseases of the stomach and intestine. PANSA 40 is used to treat adults and adolescents 12 years of age and above for
• Reflux oesophagitis. An inflammation of your oesophagus (the tube which connects your throat to your stomach) accompanied by the regurgitation of stomach acid. PANSA 40 is used to treat adults for
• An infection with a bacterium called Helicobacter pylori in patients with duodenal ulcers and stomach ulcers in combination with two antibiotics (eradication therapy). The aim is to get rid of the bacteria and so reduce the likelihood of these ulcers returning.
• Stomach and duodenal ulcers.
• Zollinger-Ellison Syndrome and other conditions producing too much acid in the stomach.
2. What you need to know before you take PANSA 40
Do not take PANSA 40
- If you are allergic to pantoprazole or to any of the other ingredients of this medicine (section 6).
- If you are allergic to medicines containing other proton pump inhibitors.
Warnings and precautions
Talk to your doctor before taking Pantoprazole
- If you have severe liver problems. Please tell your doctor if you have ever had problems with your liver in the past. Your doctor will check your liver enzymes more frequently, especially when you are taking Pantoprazole as a long-term treatment. In the case of a rise of liver enzymes the treatment should be stopped.
- If you have reduced body stores or risk factors for reduced vitamin B12 and receive long-term treatment with pantoprazole. As with all acid reducing agents, pantoprazole may lead to a reduced absorption of vitamin B12.
- If you are taking HIV protease inhibitors such as atazanavir (for the treatment of HIV-infection) at the same time as pantoprazole, ask your doctor for specific advice.
- Taking a proton pump inhibitor like pantoprazole, especially over a period of more than one year, may slightly increase your risk of fracture in the hip, wrist or spine. Tell your doctor if you have osteoporosis (reduced bone density) or if you have been told that you are at risk of getting osteoporosis (for example, if you are taking steroids).
- If you are on Pantoprazole for more than three months it is possible that the levels of magnesium in your blood may fall. Low levels of magnesium can be seen as fatigue, involuntary muscle contractions, disorientation, convulsions, dizziness, increased heart rate. If you get any of these symptoms, please tell your doctor promptly. Low levels of magnesium can also lead to a reduction in potassium or calcium levels in the blood. Your doctor may decide to perform regular blood tests to monitor your levels of magnesium.
- If you have ever had a skin reaction after treatment with a medicine similar to Pantoprazole that reduces stomach acid.
- If you get a rash on your skin, especially in areas exposed to the sun tell your doctor as soon as you can, as you may need to stop your treatment with Pantoprazole. Remember to also mention any other ill-effects like pain in your joints.
- if you are due to have a specific blood test (Chromogranin A).
Tell your doctor immediately, before or after taking this medicine, if you notice any of the following
symptoms, which could be a sign of another, more serious, disease:
- an unintentional loss of weight
- vomiting, particularly if repeated
- vomiting blood; this may appear as dark coffee grounds in your vomit
- you notice blood in your stools; which may be black or tarry in appearance
- difficulty in swallowing or pain when swallowing
- you look pale and feel weak (anaemia)
- chest pain
- stomach pain
- severe and/or persistent diarrhoea, because this medicine has been associated with a small increase in infectious diarrhoea.
Your doctor may decide that you need some tests to rule out malignant disease because pantoprazole also alleviates the symptoms of cancer and could cause delay in diagnosing it. If your symptoms continue in spite of your treatment, further investigations will be considered. If you take Pantoprazole on a long-term basis (longer than 1 year) your doctor will probably keep you under regular surveillance. You should report any new and exceptional symptoms and circumstances whenever you see your doctor.
Children and adolescents
PANSA 40 is not recommended for use in children as it has not been proven to work in children below 12 years of age.
Other medicines and PANSA 40
Tell your doctor if you are taking, have recently taken or might take any other medicines, including medicines obtained without a prescription. This is because Pantoprazole may influence the effectiveness of other medicines, so tell your doctor if you are taking:
- Medicines such as ketoconazole, itraconazole and posaconazole (used to treat fungal infections) or erlotinib (used for certain types of cancer) because Pantoprazole may stop these and other medicines from working properly.
- Warfarin and phenprocoumon, which affect the thickening, or thinning of the blood. You may need further checks.
- Medicines used to treat HIV-infection, such as atazanavir.
- Methotrexate (used to treat rheumatoid arthritis, psoriasis, and cancer)
– if you are taking methotrexate your doctor may temporarily stop your Pantoprazole treatment because pantoprazole can increase levels of methotrexate in the blood.
- Fluvoxamine (used to treat depression and other psychiatric diseases)
– if you are taking fluvoxamine your doctor may reduce the dose.
- Rifampicin (used to treat infections).
- St John’s wort (Hypericum perforatum) (used to treat mild depression).
Pregnancy and breast-feeding and fertility
There are no adequate data from the use of pantoprazole in pregnant women. Excretion into human milk has been reported. If you are pregnant or breast-feeding, think you may be pregnant, or are planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine. You should use this medicine, only if your doctor considers the benefit for you greater than the potential risk for your unborn child or baby.
Driving and using machines
PANSA 40 has no or negligible influence on the ability to drive and use machines. If you experience side effects like dizziness or disturbed vision, you should not drive or operate machines.
PANSA 40 contains sodium
This medicine contains less than 1 mmol sodium (23 mg) per tablet, that is to say essentially ‘sodium-free’.
3. How to take PANSA 40
Always take this medicine exactly as your doctor or pharmacist has told you. Check with your doctor or pharmacist if you are not sure.
Method of administration
Take the tablets 1 hour before a meal without chewing or breaking them and swallow them whole with some water. The recommended dose is:
Adults and adolescents 12 years of age and above
To treat reflux oesophagitis
The usual dose is one tablet a day. Your doctor may tell you to increase to 2 tablets daily. The treatment period for reflux oesophagitis is usually between 4 and 8 weeks. Your doctor will tell you how long to take your medicine.
Adults
For the treatment of an infection with a bacterium called Helicobacter pylori in patients with duodenal ulcers and stomach ulcers in combination with two antibiotics (Eradication therapy).
One tablet, two times a day plus two antibiotic tablets of either amoxicillin, clarithromycin and metronidazole (or tinidazole), each to be taken two times a day with your pantoprazole tablet. Take the first pantoprazole tablet 1 hour before breakfast and the second pantoprazole tablet 1 hour before your evening meal. Follow your doctor’s instructions and make sure you read the package leaflets for these antibiotics. The usual treatment period is one to two weeks.
For the treatment of stomach and duodenal ulcers.
The usual dose is one tablet a day. After consultation with your doctor, the dose may be doubled. Your doctor will tell you how long to take your medicine. The treatment period for stomach ulcers is usually between 4 and 8 weeks. The treatment period for duodenal ulcers is usually between 2 and 4 weeks.
For the long-term treatment of Zollinger-Ellison-Syndrome and of other conditions in which too much stomach acid is produced.
The recommended starting dose is usually two tablets a day. Take the two tablets 1 hour before a meal. Your doctor may later adjust the dose, depending on the amount of stomach acid you produce. If prescribed more than two tablets a day, the tablets should be taken twice daily.
If your doctor prescribes a daily dose of more than four tablets a day, you will be told exactly when to stop taking the medicine.
Patients with kidney problems
If you have kidney problems, you should not take Pantoprazole for eradication of Helicobacter pylori.
Patients with liver problems
If you suffer from severe liver problems, you should not take more than one tablet 20 mg pantoprazole a day (for this purpose tablets containing 20 mg pantoprazole are available).
If you suffer from moderate or severe liver problems, you should not take Pantoprazole for eradication of Helicobacter pylori.
Use in children and adolescents
These tablets are not recommended for use in children below 12 years. If you take more Pantoprazole than you should Consult your doctor or pharmacist. There are no known symptoms of overdose.
If you forget to take PANSA 40
Do not take a double dose to make up for a forgotten dose. Take your next, normal dose at the usual time.
If you stop taking PANSA 40
Do not stop taking these tablets without first talking to your doctor or pharmacist. If you have any further questions about the use of this medicine, ask your doctor.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
If you get any of the following side effects, stop taking these tablets and tell your doctor immediately, or contact the casualty department at your nearest hospital:
- Serious allergic reactions (frequency rare: may affect up to 1 in 1,000 people): swelling of the tongue and/or throat, difficulty in swallowing, hives (nettle rash), difficulties in breathing, allergic facial swelling (Quincke’s oedema / angioedema), severe dizziness with very fast heartbeat and heavy sweating.
- Serious skin conditions (frequency not known: frequency cannot be estimated from the available data): you may notice one or more of the following - blistering of the skin and rapid deterioration of your general condition, erosion (including slight bleeding) of eyes, nose, mouth/lips or genitals, or skin sensitivity/rash, particularly in areas of skin exposed to light/the sun. You may also have joint pain or flu-like symptoms, a fever, swollen glands (e.g. in the armpit) and blood tests may show changes in certain white blood cells or liver enzymes (Stevens-Johnson Syndrome, Lyell Syndrome, Erythema multiforme, Subacute cutaneous lupus erythematosus, Drug reaction with eosinophilia and systemic symptoms (DRESS), Photosensitivity).
- Other serious conditions (frequency not known: yellowing of the skin or whites of the eyes (severe damage to liver cells, jaundice) or fever, rash, and enlarged kidneys sometimes with painful urination, and lower back pain (serious inflammation of the kidneys), possibly leading to kidney failure. Other side effects are:
- Common (may affect up to 1 in 10 people)
Benign polyps in the stomach.
- Uncommon (may affect up to 1 in 100 people)
Headache; dizziness; diarrhoea; feeling sick, vomiting; bloating and flatulence (wind); constipation; dry mouth; abdominal pain and discomfort; skin rash, exanthema, eruption; itching; feeling weak, exhausted or generally unwell; sleep disorders; fracture in the hip, wrist or spine.
- Rare (may affect up to 1 in 1,000 people)
Distortion or complete lack of the sense of taste; disturbances in vision such as blurred vision; hives; pain in the joints; muscle pains; weight changes; raised body temperature; high fever; swelling of the extremities (peripheral oedema); allergic reactions; depression; breast enlargement in males.
- Very Rare (may affect up to 1 in 10,000 people)
Disorientation.
- Not known (frequency cannot be estimated from the available data)
Hallucination, confusion (especially in patients with a history of these symptoms); feeling of tingling, prickling, pins and needles, burning sensation or numbness, rash, possibly with pain in the joints, inflammation in the large bowel, that causes persistent watery diarrhoea.
Side effects identified through blood tests:
- Uncommon (may affect up to 1 in 100 people) an increase in liver enzymes.
- Rare (may affect up to 1 in 1,000 people) an increase in bilirubin; increased fat levels in blood; sharp drop in circulating granular white blood cells, associated with high fever.
- Very Rare (may affect up to 1 in 10,000 people) a reduction in the number of blood platelets, which may cause you to bleed or bruise more than normal; a reduction in the number of white blood cells, which may lead to more frequent infections; coexisting abnormal reduction in the number of red and white blood cells, as well as platelets.
- Not known (frequency cannot be estimated from the available data) decreased level of sodium, magnesium, calcium or potassium in blood (see section 2).
Reporting of side effects
If you get any side effects, talk to your doctor. This includes any possible side effects not listed in this leaflet. You can also report side effects directly: Website: www.zuventus.com and click the tab “Safety Reporting” located on the top right end of the home page. By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store PANSA 40
Keep this medicine out of the sight and reach of children. Do not use this medicine after the expiry date which is stated on the carton and the container after Exp. The expiry date refers to the last day of that month.
This medicine does not require any special storage conditions.
Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help to protect the environment.
6. Contents of the pack and other information
What PANSA 40 contains
- The active substance is pantoprazole.
- Each gastro-resistant tablet contains 40 mg of pantoprazole (as sodium).
- Excipients q.s.
- Colours: Yellow Oxide of Iron & Titanium Dioxide IP
PANSA 40 is available in the following pack sizes:
15 gastro-resistant tablets in each strip
20 Blister strips in one sale carton.