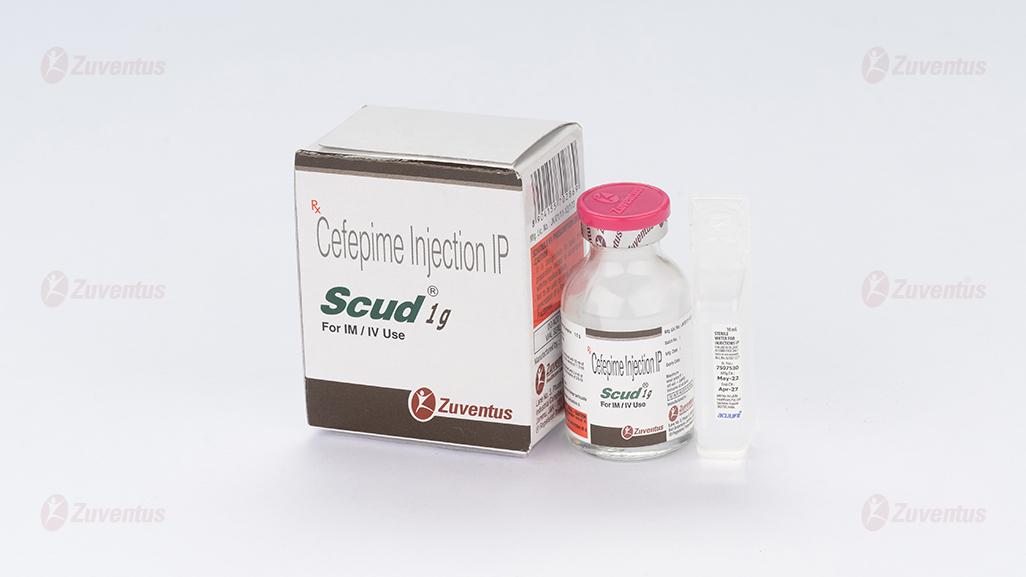
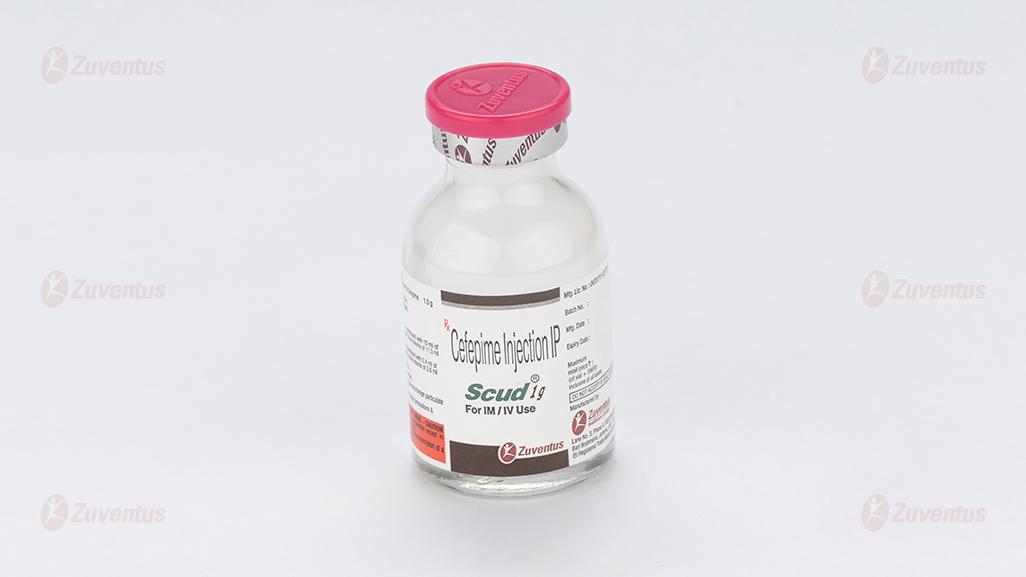
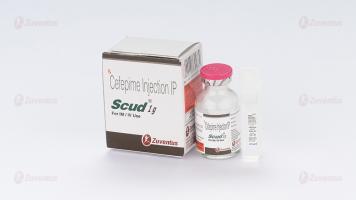
Scud Injection
Therapy Area
Anti Infective
Composition :
Scud 250 mg
Each vial contains :
Cefepime Hydrochloride IP equivalent to Cefepime 250 mg
L-Arginine IP for pH adjustment.
This pack contains Sterile Water for Injections IP 5 ml.
Scud 500 mg
Each vial contains :
Cefepime Hydrochloride IP equivalent to Cefepime 500 mg
L-Arginine IP for pH adjustment.
This pack contains Sterile Water for Injections IP 10 ml.
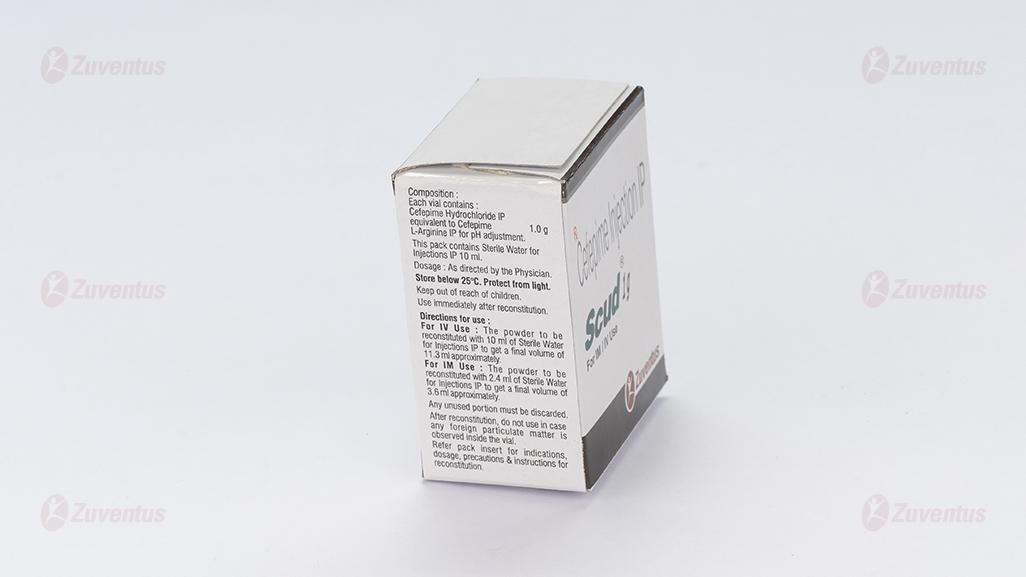
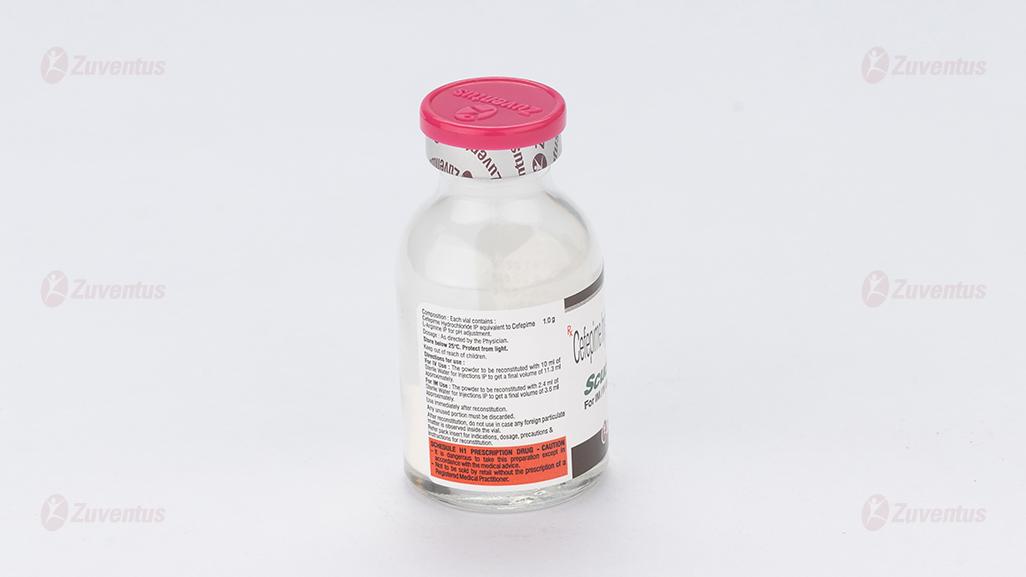
Scud 1 g
Each vial contains :
Cefepime Hydrochloride IP equivalent to Cefepime 1.0 g
L-Arginine IP for pH adjustment.
This pack contains Sterile Water for Injections IP 10 ml.
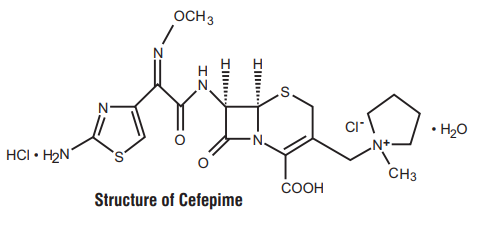
Description :
Cefepime is a semi-synthetic, broad spectrum, fourth-generation cephalosporin antibiotic for parenteral administration. It has been shown to be more effective than other third-generation cephalosporin against several gram-negative isolates with better gram-positive coverage, good antipseudomonal activity and good betalactamase stability. In addition, the drug has been shown to inhibit various Enterobacteriaceae resistant to cefotaxime and ceftazidime. The chemical name is 1-[[(6R,7R)-7-[2-(2-amino-4-thiazolyl)-glyoxylamido]- 2 carboxy-8-oxo 5-thia-1-azabicyclo [4.2.0]oct-2-en-3-yl]methyl]- 1 methylpyrrolidinium chloride, 72-(Z)-(O methyloxime), monohydrochloride, monohydrate, which corresponds to the following Structural formula :
Clinical pharmacology :
CLINICAL PHARMACOLOGY :
Pharmacodynamics :
Cefepime is bactericidal agent that acts by inhibition of bacterial cell wall synthesis. Cefepime has a broad spectrum of in vitro activity that encompasses a wide range of gram-positive and gram-negative bacteria. Cefepime is highly resistance to hydrolysis by most beta-lactamases and exhibits rapid penetration into gramnegative bacterial cells. Within bacterial cells, the molecular targets of Cefepime are the penicillin binding proteins (PBP).
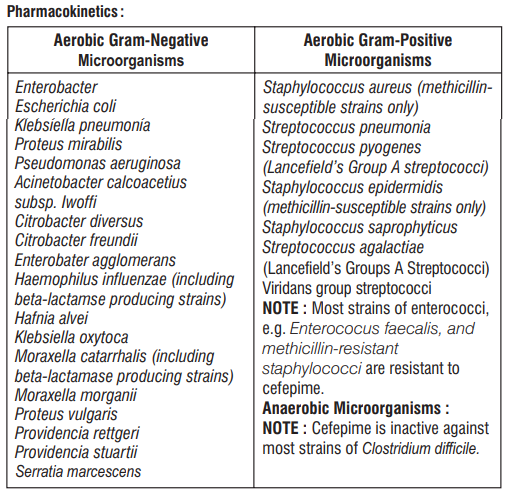
Antibacterial Spectrum :
Cefepime has been shown to be active against most strains of the following microorganisms.
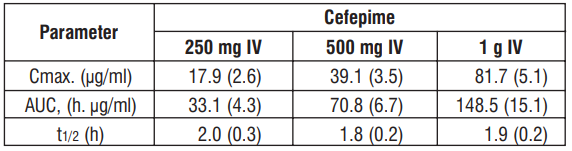
The average plasma concentrations of Cefepime observed in healthy adult male volunteers (n=9) at various times following single 30 minute infusions (IV) of Cefepime 500 mg and 1g are summarized in Table 1. Elimination of Cefepime is principally via renal excretion with an average (± SD) half-life of 2.0 (± 0.3) hours and total body clearance of 120.0 (± 8.0) mL/min in healthy volunteers. Cefepime pharmacokinetics are linear over the range 250 mg to 1 g IV. There is no evidence of accumulation. The average steady state volume of distribution of Cefepime is 18.0 (± 2.0) L. The serum protein binding of Cefepime is approximately 20 % and is independent of its concentration in serum. Cefepime is excreted unchanged in urine which accounts for approximately 85% of the administered dose.
TABLE 1
Average plasma concentrations in mg/mL of Cefepime and Derived Pharmacokinetic Parameters (± SD), on Intravenous Administration.
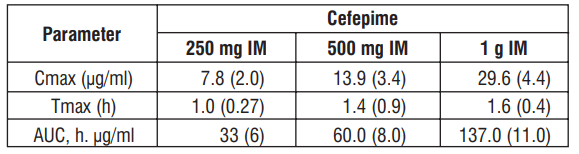
Following intramuscular (IM) administration, Cefepime is completely absorbed. The average plasma concentrations of Cefepime at various times following a single IM injection are summarized in Table 2. The pharmacokinetics of Cefepime are linear over the range of 500 mg to 1 g IM and do not vary with respect to treatment duration.
TABLE 2
Average Plasma Concentrations in mg/ml of Cefepime and Derived Pharmacokinetic Parameters (± SD), Intramuscular Administration.
Metabolism and Excretion :
Cefepime is metabolized to N-methylpyrrolidine (NMP) which is rapidly converted to the N-oxide (NMP-N-oxide). Urinary recovery of unchanged Cefepime accounts for approximately 85 % of the administered dose. Less than 1 % of the administered dose is recovered from urine as NMP, 6.8 % as NMP-N-oxide, and 2.5 % as an epimer of Cefepime. Because renal excretion is a significant pathway of elimination, patients with renal dysfunction and patients undergoing hemodialysis require dosage adjustment.
Special Populations :
Paediatric patients : No accumulation was seen when Cefepime was given at 50 mg/kg q 12 h, while Cmax, AUC, and t½ were increased about 15 % at steady state after 50 mg/kg q 8 h.
Geriatric patients : There is decrease in Cefepime total body clearance as a function of creatinine clearance. Therefore, dosage administration of Cefepime in the elderly should be adjusted as appropriate if the patients creatinine clearance is 60 ml/min or less.
Renal insufficiency : Total body clearance decreased proportionally with creatinine clearance in patients with abnormal renal function which serves as the basis of dosage adjustment recommendations in this group of patients.
Hepatic insufficiency : The pharmacokinetics of Cefepime were unaltered in patients with impaired hepatic function who received a single 1 g dose.
Indications and usage :
INDICATIONS AND USAGE :
Cefepime is indicated in the treatment of the following infections :
• Pneumonia (moderate to severe).
• Empiric Therapy for febrile Neutropenic Patients.
• Uncomplicated and complicated Urinary Tract Infections (including pyelonephritis).
• Uncomplicated Skin and Skin structure Infections.
• Complicated Intra-abdominal Infection (Used combination with metronidazole)
Culture and susceptibility testing should be performed where appropriate to determine the susceptibility of the causative microorganism(s) to Cefepime.
Dosage and Administration :
The recommended adult and paediatric dosages and routes of administration are outlined in the following Table 3. Cefepime should be administered intravenously over approximately 30 minutes.
TABLE 3
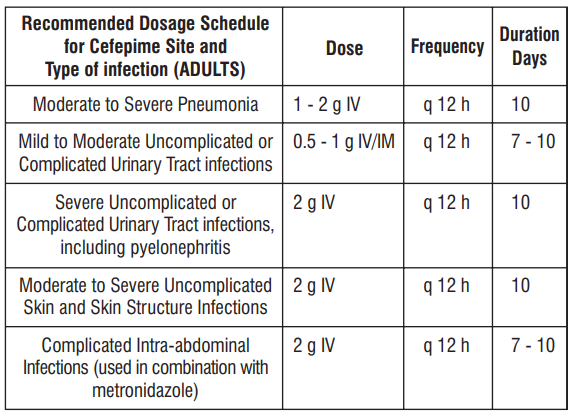
Paediatric Patients (2 months up to 16 years) :
The maximum dose for paediatric patients should not exceed the recommended adult dose.
The usual recommended dosage in paediatric patients is 50 mg/kg/dose, administered q 12 h (Q 8 h for febrile Neutropenic patients), for duration as given above or until resolution of neutropenia. In patients whose fever resolves but who remain neutropenic for more than 7 days, the need for continued antimicrobial therapy should be re-evaluated frequently.
Impaired Hepatic Function - No adjustment is necessary for patients with impaired hepatic function.
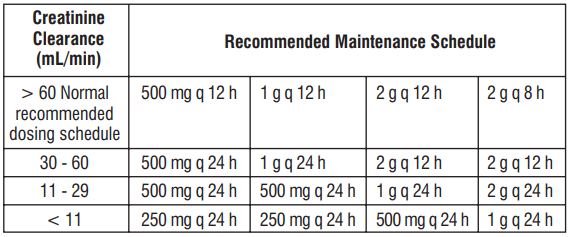
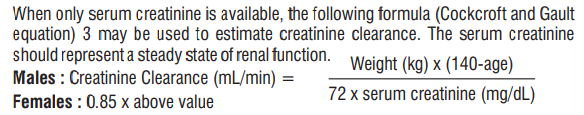
Impaired Renal Function - In patients with impaired renal function (creatinine clearance 60 mL/min), the dose of Cefepime should be adjusted to compensate for the slower rate of renal elimination. The recommended maintenance doses of Cefepime in patients with renal insufficiency are presented in Table 4.
TABLE 4
Recommended Maintenance Schedule in Adult Patients with Renal Impairment Relative to Normal Recommended Dosing Schedule.
ADMINISTRATION :
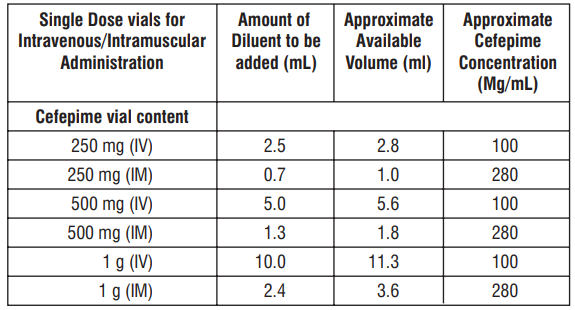
For intravenous infusion, constitute the 250 mg, 500 mg or 1 g vial, and add an appropriate quantity of resulting solution to an IV container with one of the compatible IV fluids. The resulting solution should be administered over approximately 30 minutes. Intramuscular Administration : For IM administration. Cefepime should be constituted with one of the following diluents : Sterile Water for injection, 0.9 % Sodium Chloride 5%Dextrose Injection, 0.5%or 1.0%Lidocaine Hydrochloride, or Sterile Bacteriostatic WaterforInjection.Preparation ofCefepime solutions is summarized in Table 5.
TABLE 5
Preparation of Solutions of Cefepime.
Contraindications :
Cefepime is contraindicated in patients who have shown immediate hypersensitivity reactions to Cefepime or the cephalosporin class of antibiotics, penicillins or other beta-lactam antibiotics
Warnings :
Before therapy with cefepime is instituted, careful inquiry should be made to determine whether the patient has had previous immediate hypersensitivity reactions to Cefepime, cephalosporins, penicillins, or other drugs. If this product is to be given to penicillin-sensitive patients, caution should be exercised because crosshypersensitivity among beta-lactam antibiotics has been clearly documented and may occur in up to 10 % of patients with a histor y of penicillin allergy. If an allergic reaction to Cefepime occurs, discontinue the drug. Serious acute hypersensitivity reactions may require treatment with epinephrine and other emergency measures including oxygen, corticosteroids, intravenous fluids, intravenous antihistamines, pressor amines, and airway management, as clinically indicated. Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including Cefepime for injection, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
Precautions :
General :
• In patients with creatinine clearance less than or equal to 60 mL/min, the dose of cefepime (Cefepime hydrochloride) should be adjusted to compensate for the slower rate of renal elimination.
• Prothrombin time should be monitored.
• Positive direct Coombs test have been reported during treatment with Cefepime.
• Caution should be exercised in individuals with a history of gastrointestinal disease, particularly colitis.
Drug interactions :
Renal function should be monitored carefully if high does of aminoglycosides are to be administered with Cefepime because of the increased potential of nephrotoxicity and ototoxicity of aminoglycoside antibiotics. Nephrotoxicity has been reported following concomitant administration of other cephalosporins with potent diuretics such as furosemide.
Drug/Laboratory Test Interactions :
The administration of Cefepime may result in a false-positive reaction for glucose in the urine when using clinitest tablets. It is recommended that glucose tests based on enzymatic glucose oxidase reactions (such as Clinistix or Test-Tape) be used.
Carcinogenesis, Mutagenesis, and Impairment of Fertility :
Tests for genetic toxicity indicated no definitive evidence of genotoxic potential.
Usage in Pregnancy : Teratogenic effects-Pregnancy Category B :
No adequate and well-controlled studies of Cefepime’s use in pregnant women are available. Drug should be used during pregnancy only if clearly needed.
Nursing Mothers :
Cefepime is excreted in human breast milk in very low concentrations (0.5 mg/ml). Caution should be exercised when Cefepime is administered to a nursing woman.
Paediatric Use :
The safety and effectiveness of Cefepime has been established in the age group ranging from 2 months upto 16 years. Safety and effectiveness in paediatric patients below the age of 2 months have not been established.
Geriatric Use :
When geriatric patients received the usual recommended adult dose, clinical efficacy and safety were comparable to clinical efficacy and safety in nongeriatric adult patients. Serious adverse events have occurred in geriatric patients with renal insufficiency given unadjusted doses of Cefepime. Elderly patients are more likely to have decreased renal function, and so care should be taken in dose selection, and renal function should be monitored.
Adverse Reactions :
In clinical trials using multiple doses of Cefepime, 4137 patients were treated with the recommended dosages of Cefepime (500 mg to 2 g IV q 12 h). The adverse reactions were local reactions (3.0 %) including phlebitis (1.3 %) pain and/or inflammation (0.6 %); rash (1.1 %).
Less frequent were Colitis (including pseudomembranous colitis), diarrhea, fever, headache, nausea, oral moniliasis, pruritus, urticaria, vaginitis, vomiting. As with other cephalosporins, anaphylaxis including anaphylactic shock transient leucopenia, neutropenia, agranulocytosis and thrombocytopenia have been reported. Cephalosporin-class adverse reactions :
In addition to the adverse reactions listed above that have been observed in patients treated with Cefepime, the following adverse reactions and altered laboratory tests have been reported for cephalosporin class antibiotics : Stevens-johnson syndrome, erythema multiforme : toxic epidermal necrolysis, renal dysfunction, toxic nephropathy, aplastic anemia, hemolytic anemia, hemorrhage, hepatic dysfunction including cholestasis and pancytopenia.
Overdosage :
Patients who receive an overdose should be carefully observed and given supportive treatment. In the presence of renal insufficiency, hemodialysis, not peritoneal dialysis, is recommended to aid in the removal of Cefepime from the body. Symptoms of overdose include encephalopathy (disturbance of consciousness including confusion, hallucinations, stupor and coma) myoclonus, seizures and neuromuscular excitability.
Compatibility and Stability :
Intravenous : Cefepime is compatible at concentrations between 1 and 40 mg/mL with the following IV infusion fluids : 0.9 % Sodium Chloride Injection, 5 % and 10 % Dextrose Injection, M/6 Sodium Lactate Injection, 5 % Dextrose and 0.9 % Sodium Chloride Injection, Lactated Ringers and 5 % Dextrose Injection. These solutions may be stored upto 24 hours at controlled room temperature 20°- 25° C (68°- 77° F) or 7 days in a refrigerator 2°- 8°C (36° – 46°F). Cefepime vials is stable at concentrations of 10 - 40 mg/mL in 5 % Dextrose Injection or 0.9 % Sodium Chloride Injection for 24 hours at controlled room temperature 20°- 25°C or 7 days in a refrigerator 2°- 8°C. Cefepime admixture compatibility information is summarized in Table 6.
TABLE 6
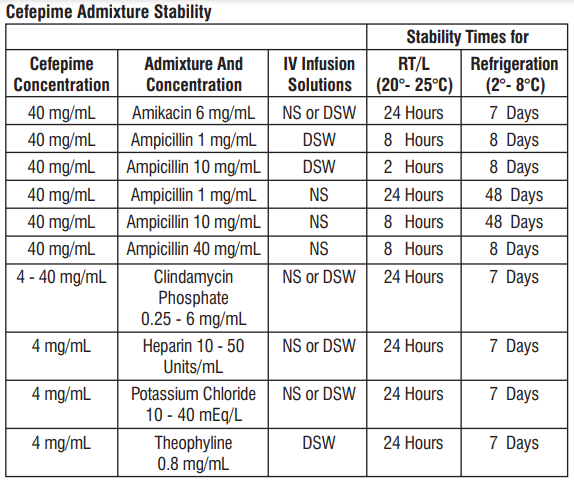
NS = 0.9 % Sodium Chloride Injection
DSW=5 % Dextrose Injection.
RT/L = Ambient room temperature and light
Solutions of Cefepime, like those of most beta-lactam antibiotics, should not be added to solutions of ampicillin at a concentration greater than 40 mg/mL, and should not be added to metronidazole, vancomycin, gentamicin, tobramycin, netilmicin sulfate or aminophylline because of potential interaction. However, if concurrent therapy with Cefepime is indicated, each of these antibiotics can be administered separately. Intramuscular : Cefepime constituted as directed is stable for 24 hours at controlled room temperature 20°- 25°C (68°- 77°F) or for 7 days in a refrigerator 2°- 8°C (36°- 46°F) with the following diluents : Sterile Water for injection, 0.9 % Sodium Chloride Injection, 5 % Dextrose Injection. Sterile Bacteriostatic Water for Injection with Parabens or Benzyl Alcohol, or 0.5 % or 1 % Lidocaine Hydrochloride.
Storage :
STORAGE :
Store below 25°C. Protect from light.
Keep out of reach of children
After reconstitution, do not use in case any foreign particulate matter is observed inside the vial.
Presentation :
Scud 250 mg : A vial of 250 mg with SWFI IP 5 ml.
Scud 500 mg : A vial of 500 mg with SWFI IP 10 ml.
Scud 1 g : A vial of 1.0 g with SWFI IP 10 ml.
Read all of this leaflet carefully before you start using this medicine because it contains important information for you.
-Keep this leaflet. You may need to read it again.
-If you have any further questions, ask your doctor, pharmacist or nurse.
-This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
-If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
What is in this leaflet
1. What Scud is and what it is used for
2. What you need to know before you use Scud
3. How to use Scud
4. Possible side effects
5. How to store Scud
6. Contents of the pack and other information
1. What Scud is and what it is used for
Scud is indicated in the treatment of infections caused by bacteria susceptible to cefepime, namely:
- lower respiratory tract infections, including nosocomial pneumonia and community-acquired pneumonia, acute bacterial exacerbation of chronic bronchitis and secondary bacterial infection of acute bronchitis;
- uncomplicated and complicated urinary tract infections, including pyelonephritis;
- skin and subcutaneous tissue infection;
- intrabdominal infection, including peritonitis, and biliary tract infections;
- gynecological infections;
- bacterial meningitis in infants and children;
- in combination with other antibacterial agents in the management of neutropenic patients with fever that is suspected to be due to a bacterial infection;
- treatment of patients with bacteraemia that occurs in association with, or is suspected to be associated with, any of the infections listed above.
Consideration should be given to official guidance on the appropriate use of antibacterial agents.
2. What you need to know before you use Scud
Do not use Scud:
- if you are allergic to cefepime, any other cephalosporin antibiotics or any of the other ingredients of this medicine (listed in section 6).
- if you have a history of severe allergic reaction any other type of beta-lactam antibiotics (penicillins, monobactams and carbapenems).
Warnings and precautions
Talk to your doctor, pharmacist or nurse before using Scud.
Particular care should be taken when using Scud:
– Severe and occasionally fatal allergic reactions were reported. Please tell your doctor if you have a history of asthma or allergic reactions (skin rash, itching…). Severe allergic reactions may need epinephrine and other support therapy.
– Cefepime is not adequate for the treatment of certain types of infections. Your doctor has prescribed you this antibiotic because it is the best option for your illness.
– if you have kidney problems (such as reduced renal function) as the elimination of this medicine may be affected.
– if you suffer from persistent diarrhoea during or after using this medicine. Tell your doctor immediately so he can investigate whether the diarrhoea is the result of an intestinal inflammation caused by the use of the antibiotic; treatment with this medicine may need to be discontinued.
– If you suffer from allergies (such as hay fever, nettle rash) or have had an allergic reaction to medicines in the past.
Cefepime must be discontinued on the appearance of any kind of hypersensitivity reaction and appropriate therapeutic measures initiated.
– Dosages for elderly patients should be chosen carefully and should take renal function into account, as there is a greater possibility to develop kidney disease.
Other medicines and Scud
Tell your doctor or pharmacist if you are using, have recently used or might use any other medicines, including medicines obtained without prescription.
Renal function should be carefully monitored when Scud is combined with drugs that may affect the kidneys (such as aminoglycosides and powerful diuretics).
The cephalosporins may enhance the effect of coumarin anticoagulants.
Interaction with diagnostic tests
Cefepime may produce a false positive reaction in some laboratory tests (urine glucose and Coombs test results).
Pregnancy and breast-feeding
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for
advice before using this medicine.
Do not use this medicine during pregnancy, unless absolutely necessary and specifically directed by your doctor. If you get pregnant during treatment with Scud tell your doctor.
Scud can be transferred to breast milk, therefore this medicine should be used during breast-feeding with great care and only after discussing with your doctor.
Driving and using machines
There have been no studies on the effects on the ability to drive and use machines.
However, you may experience disturbed consciousness, dizziness, confusion and hallucination, which may compromise the ability to drive and use machines.
3. How to use Scud
Always use this medicine exactly as your doctor or pharmacist has told you. Check with your doctor or pharmacist if you are not sure.
The usual dose and the route of administration vary in accordance with the severity of the infection, the renal function, and the general conditions of the patient.
For adult patients and children with a body weight > 40 kg, with normal renal function:
|
Severity of the infection |
Dosage and route of administration |
Interval between doses |
|
Mild to moderate urinary tract infections (UTI) |
500 mg to 1 g of cefepime, IV or IM |
every 12 h |
|
Other mild to moderate infections (non-UTI) |
1g of cefepime, IV or IM |
every 12 h |
|
Severe infections |
2g of cefepime, IV |
every 12 h |
|
Very severe infection or life-threatening infections |
2g of cefepime, IV |
every 8 h |
The usual duration of treatment is 7 to 10 days; more serious infections may require a longer treatment. In the empiric treatment of febrile neutropenia, the usual treatment duration should not be less than 7 days or until the resolution of the neutropenia. In patients with a body weight ≤ 40 kg, the recommended dosage for children applies.
Use in children
For children with normal renal function:
In children the recommended dose is:
– Pneumonia, urinary tract infections, skin and subcutaneous tissue infection:
- Children aged more than 2 months and weighing ≤ 40 kg: 50 mg/kg every 12 hours for 10 days; in more severe infections, the 8 hours interval between the intakes should be done.
– Bacteraemia that occurs in association with, or is suspected to be associated infections, bacterial meningitis and empirical treatment of febrile neutropenia:
- Children aged more than 2 months and weighing ≤ 40 kg: 50 mg/kg every 8 hours during 7 to 10 days.
Experience in children under 2 months of age is limited. Children of this age should be monitored carefully during administration of Scud.
In children with body weight > 40 kg, the adult dosage is recommended.
Do not exceed the maximum recommended adult dose (2 g of cefepime every 8 hours). Experience with the intramuscular route in children is limited.
Elderly, patients with renal dysfunction, dialysis patients and children with renal dysfunction:
The doctor will determine the dose to be administered.
If you use more Scud than you should
Contact your doctor or other healthcare professionals immediately, as you may experience more severe side effects under certain situations.
If you have any further questions on the use of this medicine, ask your doctor, pharmacist or nurse.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them. Scud may present one or more of the following side effects:
Very common (can affect more than 1 user in 10):
- Positive Coombs test without hemolysis (method of determining antibody levels);
Common (can affect up to 1 user in 10):
- Increased blood coagulation time (increased prothrombin or thromboplastin time);
- anaemia;
- an elevated level of certain blood cells (eosinophilia);
- infusion site phlebitis;
- diarrhoea;
- rashes;
- infusion site reaction;
- pain and inflammation on the injection site;
- an elevated level in certain blood counts (alanine aminotransferase, aspartate aminotransferase, bilirubin, alkaline phosphatase).
Uncommon (can affect up to 1 user in 100)
- fungal infections of the mouth with white coating (oral candidiasis);
- vaginal infection;
- reduced levels of certain blood cells (thrombocytopenia, leukopenia, neutropenia)
- headaches;
- colitis (inflammation of the large intestine);
- pseudomembranous colitis;
- nausea;
- vomiting;
- erythema (reddening of the skin);
- urticaria;
- itching;
- elevated blood urea;
- elevated serum creatinine;
- fever;
- inflammation on the infusion site.
Rare (can affect up to 1 user in 1,000):
- fungal infections (candidiasis);
- allergic reactions;
- angioedema (sudden swelling of the skin, subcutaneous tissue, mucosa or submucosa);
- convulsions;
- tingling;
- taste changes;
- dizziness;
- vascular dilation;
- shortness of breath;
- abdominal pain;
- constipation;
- genital itching;
- chills.
Not known (unknown frequency)
- aplastic anaemia, haemolytic anaemia e agranulocytosis;
- confusion;
- hallucinations;
- coma;
- torpidity;
- encephalopathy (non-inflammatory brain disease)
- disturbed consciousness;
- myoclonus (muscle twitching);
- bleeding;
- gastrointestinal disease;
- severe skin reactions (as toxic epidermal necrolysis, Stevens-Johnson syndrome and erythema multiforme);
- renal failure;
- toxic nephropathy (kidney damage);
- false positive urine glucose test results.
Reporting of side effects
If you get any side effects, talk to your doctor. This includes any possible side effects not listed in this leaflet. You can also report side effects directly: Website: www.zuventus.co.in and click the tab “Safety Reporting” located on the top right end of the home page.
By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Scud
Keep this medicine out of the sight and reach of children.
Do not use this medicine after the expiry date which is stated on the packaging and the container, after ‘EXP.’. The expiry date refers to the last day of that month.
This medicinal product does not require any special temperature storage conditions. Keep the container in the outer carton.
Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help protect the environment.
6. Contents of the pack and other information
What Scud contains
- The active substance is cefepime dihydrochloride monohydrate.
Scud 250 mg
Each vial contains :
Cefepime Hydrochloride IP equivalent to Cefepime 250 mg
L-Arginine IP for pH adjustment.
This pack contains Sterile Water for Injections IP 5 ml.
Scud 500 mg
Each vial contains :
Cefepime Hydrochloride IP equivalent to Cefepime 500 mg
L-Arginine IP for pH adjustment.
This pack contains Sterile Water for Injections IP 10 ml.
Scud 1 g
Each vial contains :
Cefepime Hydrochloride IP equivalent to Cefepime 1.0 g
L-Arginine IP for pH adjustment.
This pack contains Sterile Water for Injections IP 10 ml.
Pack size/ presentation:
Scud 250 mg: A vial of 250 mg with SWFI IP 5 ml.
Scud 500 mg: A vial of 500 mg with SWFI IP 10 ml.
Scud 1 g: A vial of 1.0 g with SWFI IP 10 ml.
Marketing Authorization Holder and Manufacturer
Zuventus Healthcare Limited
Zuventus House, Plot Y2, CTS No.: 358/A2,
Near Nahur Railway Station,
Nahur (W), Mumbai, 400078 Maharashtra, India.
This leaflet was last revised on 06/2023.