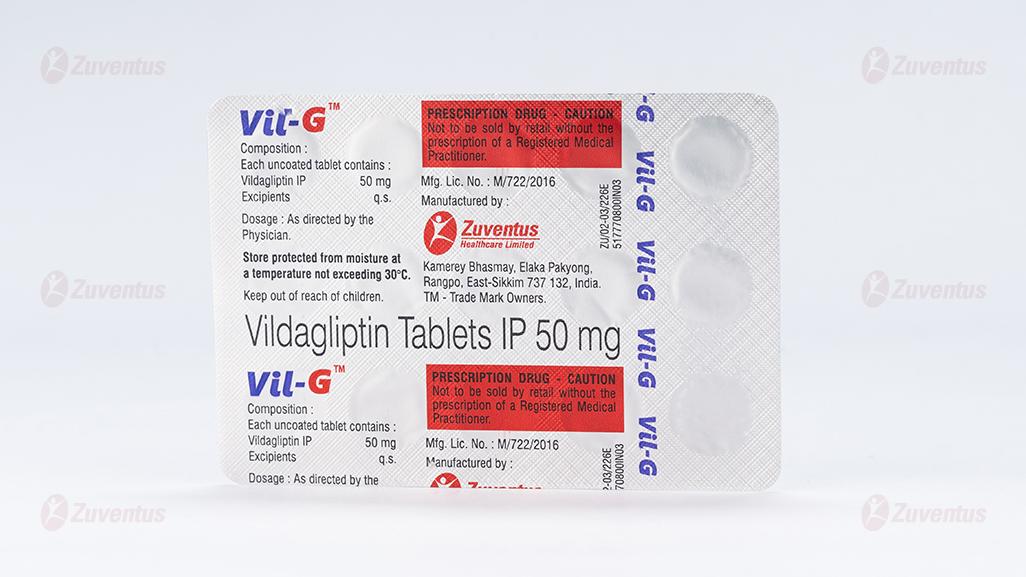
Vil G Tablets
Therapy Area
Anti-diabetic
1.0 Generic name
Vildagliptin Tablets IP 50 mg
2.0 Qualitative and quantitative composition
Each uncoated tablet contains :
Vildagliptin IP 50 mg
Excipients q.s.
3.0 Dosage form and strength
Tablet
4.0 Clinical particulars
4.1 Therapeutic indication
As an adjunct to diet and exercise to improve glycemic control in patients with type-II diabetes mellitus
4.2 Posology and method of administration Adults
When used as monotherapy, in combination with metformin, in combination with thiazolidinedione, in combination with metformin and a sulphonylurea, or in combination with insulin (with or without metformin), the recommended daily dose of Vildagliptin is 100 mg, administered as one dose of 50 mg in the morning and one dose of 50 mg in the evening.
When used in dual combination with a sulphonylurea, the recommended dose of Vildagliptin is 50 mg once daily administered in the morning. In this patient population, Vildagliptin 100 mg daily was no more effective than Vildagliptin 50 mg once daily.
When used in combination with a sulphonylurea, a lower dose of the sulphonylurea may be considered to reduce the risk of hypoglycaemia.
Doses higher than 100 mg are not recommended.
If a dose of Vildagliptin missed, it should be taken as soon as the patient remembers. A double dose should not be taken on the same day.
The safety and efficacy of Vildagliptin as triple oral therapy in combination with metformin and a thiazolidinedione have not been established.
Additional information on special populations Elderly (≥ 65 years)
No dose adjustments are necessary in elderly patients.
Renal impairment
No dose adjustment is required in patients with mild renal impairment (creatinine clearance ≥ 50 ml/min). In patients with moderate or severe renal impairment or with end-stage renal disease (ESRD), the recommended dose of Vildagliptin is 50 mg once daily
Hepatic impairment
Vildagliptin should not be used in patients with hepatic impairment, including patients with pre-treatment alanine aminotransferase (ALT) or aspartate aminotransferase (AST) > 3x the upper limit of normal (ULN).
Paediatric population
Vildagliptin is not recommended for use in children and adolescents (< 18 years). The safety and efficacy of Vildagliptin in children and adolescents (< 18 years) have not been established. No data are available.
Method of administration
Vildagliptin can be administered with or without a meal.
4.3 Contraindications
Hypersensitivity to the active substance or to any of the excipients
4.4 Special warnings and precautions for use
- General
Vildagliptin is not a substitute for insulin in insulin-requiring patients. Vildagliptin should not be used in patients with type 1 diabetes or for the treatment of diabetic ketoacidosis.
- Renal impairment
There is limited experience in patients with ESRD on haemodialysis. Therefore, Vildagliptin should be used with caution in these patients.
- Hepatic impairment
Vildagliptin should not be used in patients with hepatic impairment, including patients with pre-treatment ALT or AST > 3x ULN.
- Liver enzyme monitoring
Rare cases of hepatic dysfunction (including hepatitis) have been reported. In these cases, the patients were generally asymptomatic without clinical sequelae and liver function test results returned to normal after discontinuation of treatment. Liver function tests should be performed prior to the initiation of treatment with Vildagliptin in order to know the patient's baseline value. Liver function should be monitored during treatment with Vildagliptin at three-month intervals during the first year and periodically thereafter. Patients who develop increased transaminase levels should be monitored with a second liver function evaluation to confirm the finding and be followed thereafter with frequent liver function tests until the abnormality(ies) return(s) to normal. Should an increase in AST or ALT of 3x ULN or greater persist, withdrawal of Vildagliptin therapy is recommended.
Patients who develop jaundice or other signs suggestive of liver dysfunction should discontinue Vildagliptin. Following withdrawal of treatment with Vildagliptin and LFT normalisation, treatment with Vildagliptin should not be reinitiated.
- Cardiac failure
A clinical trial of Vildagliptin in patients with New York Heart Association (NYHA) functional class I-III showed that treatment with Vildagliptin was not associated with a change in leftventricular function or worsening of pre-existing congestive heart failure (CHF) versus placebo. Clinical experience in patients with NYHA functional class III treated with Vildagliptin is still limited and results are inconclusive. There is no experience of Vildagliptin use in clinical trials in patients with NYHA functional class IV and therefore use is not recommended in these patients.
- Skin disorders
Skin lesions, including blistering and ulceration have been reported in extremities of monkeys in non-clinical toxicology studies. Although skin lesions were not observed at an increased incidence in clinical trials, there was limited experience in patients with diabetic skin complications. Furthermore, there have been post-marketing reports of bullous and exfoliative skin lesions. Therefore, in keeping with routine care of the diabetic patient, monitoring for skin disorders, such as blistering or ulceration, is recommended.
- Acute pancreatitis
Use of Vildagliptin has been associated with a risk of developing acute pancreatitis. Patients should be informed of the characteristic symptom of acute pancreatitis. If pancreatitis is suspected, Vildagliptin should be discontinued; if acute pancreatitis is confirmed, Vildagliptin should not be restarted. Caution should be exercised in patients with a history of acute pancreatitis
- Hypoglycaemia
Sulphonylureas are known to cause hypoglycaemia. Patients receiving Vildagliptin in combination with a sulphonylurea may be at risk for hypoglycaemia. Therefore, a lower dose of sulphonylurea may be considered to reduce the risk of hypoglycaemia.
4.5 Drugs interactions
- Vildagliptin has a low potential for interactions with co-administered medicinal products. Since Vildagliptin is not a cytochrome P (CYP) 450 enzyme substrate and does not inhibit or induce CYP 450 enzymes, it is not likely to interact with active substances that are substrates, inhibitors or inducers of these enzymes.
- Combination with Pioglitazone, Metformin and Glyburide Results from studies conducted with these oral antidiabetics have shown no clinically relevant pharmacokinetic interactions.
- Digoxin (Pgp substrate), Warfarin (CYP2C9 substrate) Clinical studies performed with healthy subjects have shown no clinically relevant pharmacokinetic interactions. However, this has not been established in the target population.
- Combination with Amlodipine, Ramipril, Valsartan or Simvastatin Drug-drug interaction studies in healthy subjects were conducted with Amlodipine, Ramipril, Valsartan and Simvastatin. In these studies, no clinically relevant pharmacokinetic interactions were observed after co-administration with Vildagliptin.
- Combination with ACE-inhibitors
There may be an increased risk of angioedema in patients concomitantly taking ACEinhibitors.
- As with other oral antidiabetic medicinal products the hypoglycaemic effect of Vildagliptin may be reduced by certain active substances, including Thiazides, Corticosteroids, Thyroid products and Sympathomimetics.
4.6 Use in special populations
Pregnancy
- There are no adequate data from the use of Vildagliptin in pregnant women. Studies in animals have shown reproductive toxicity at high doses. The potential risk for humans is unknown. Due to lack of human data, Vildagliptin should not be used during pregnancy.
Nursing mothers
- It is unknown whether Vildagliptin is excreted in human milk. Animal studies have shown excretion of Vildagliptin in milk. Vildagliptin should not be used during breast-feeding.
Fertility
- No studies on the effect on human fertility have been conducted for Vildagliptin
4.7 Effects on ability to drive and use machines
No studies on the effects on the ability to drive and use machines have been performed. Patients who experience dizziness as an adverse reaction should avoid driving vehicles or using machines.
4.8 Undesirable effects
Adverse reactions reported in patients who received Vildagliptin 100 mg daily as monotherapy in double-blind studies (N =1,855) The following undesirable effects have occurred Very common (> 1/10), common (> 1/100, < 1/10), uncommon (> /1000, < 1/100), rare (> 1/10,000 < 1/1000), very rare (< 1/10,000), not known (cannot be estimated from the available data).
- Infections and infestations
Very rare - Upper respiratory tract infection
Very rare - Nasopharyngitis
- Metabolism and nutrition disorders
Uncommon - Hypoglycaemia
- Nervous system disorders
Common - Dizziness
Uncommon - Headache
- Vascular disorders
Uncommon - Oedema peripheral
- Gastrointestinal disorders
Uncommon - Constipation
- Musculoskeletal and connective tissue disorders
Uncommon - Arthralgia
In addition, in controlled monotherapy trials with Vildagliptin the overall incidence of withdrawals due to adverse reactions was no greater for patients treated with Vildagliptin at doses of 100 mg daily (0.3%) than for placebo (0.6%) or comparators (0.5%). In comparative controlled monotherapy studies, hypoglycaemia was uncommon, reported in 0.4% (7 of 1,855) of patients treated with Vildagliptin 100 mg daily compared to 0.2% (2 of 1,082) of patients in the groups treated with an active comparator or placebo, with no serious or severe events reported.
In clinical trials, weight did not change from baseline when Vildagliptin 100 mg daily was administered as monotherapy (-0.3 kg and -1.3 kg for Vildagliptin and placebo, respectively). Clinical trials of up to 2 years' duration did not show any additional safety signals or unforeseen risks with Vildagliptin monotherapy
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via email to : medico@zuventus.com Website : https://www.zuventus.com/drug-safety-reporting
4.9 Overdose
Information regarding overdose with Vildagliptin is limited.
Symptoms
Information on the likely symptoms of overdose was taken from a rising dose tolerability study in healthy subjects given Vildagliptin for 10 days. At 400 mg, there were three cases of muscle pain, and individual cases of mild and transient paraesthesia, fever, oedema and a transient increase in lipase levels. At 600 mg, one subject experienced oedema of the feet and hands, and increases in creatine phosphokinase (CPK), aspartate aminotransferase (AST), C-reactive protein (CRP) and myoglobin levels. Three other subjects experienced oedema of the feet, with paraesthesia in two cases. All symptoms and laboratory abnormalities resolved without treatment after discontinuation of the study medicinal product.
Management
In the event of an overdose, supportive management is recommended. Vildagliptin cannot be removed by haemodialysis. However, the major hydrolysis metabolite (LAY 151) can be removed by haemodialysis.
5.0 Pharmacological properties
5.1 Mechanism of action
The administration of Vildagliptin results in a rapid and complete inhibition of DPP-4 activity, resulting in increased fasting and postprandial endogenous levels of the incretin hormones GLP-1 (Glucagon-Like Peptide 1) and GIP (Glucose-dependent Insulinotropic Polypeptide).
5.2 Pharmacodynamic properties
By increasing the endogenous levels of these incretin hormones, Vildagliptin enhances the sensitivity of beta cells to glucose, resulting in improved glucose-dependent insulin secretion. Treatment with Vildagliptin 50 - 100 mg daily in patients with type 2 diabetes significantly improved markers of beta cell function including HOMA-β (Homeostasis Model Assessment-β), proinsulin to insulin ratio and measures of beta cell responsiveness from the frequently-sampled meal tolerance test. In non-diabetic (normal glycaemic) individuals, Vildagliptin does not stimulate insulin secretion or reduce glucose levels. By increasing endogenous GLP-1 levels, Vildagliptin also enhances the sensitivity of alpha cells to glucose, resulting in more glucose-appropriate glucagon secretion. The enhanced increase in the insulin/glucagon ratio during hyperglycaemia due to increased incretin hormone levels results in a decrease in fasting and postprandial hepatic glucose production, leading to reduced glycaemia. The known effect of increased GLP-1 levels delaying gastric emptying is not observed with Vildagliptin treatment.
5.3 Pharmacokinetic properties
Absorption
Following oral administration in the fasting state, Vildagliptin is rapidly absorbed, with peak plasma concentrations observed at 1.7 hours. Food slightly delays the time to peak plasma concentration to 2.5 hours, but does not alter the overall exposure (AUC). Administration of Vildagliptin with food resulted in a decreased Cmax (19%). However, the magnitude of change is not clinically significant, so that Vildagliptin can be given with or without food. The absolute bioavailability is 85%.
Distribution
The plasma protein binding of Vildagliptin is low (9.3%) and Vildagliptin distributes equally between plasma and red blood cells. The mean volume of distribution of Vildagliptin at steadystate after intravenous administration (Vss) is 71 litres, suggesting extravascular distribution.
Biotransformation
Metabolism is the major elimination pathway for Vildagliptin in humans, accounting for 69% of the dose. The major metabolite (LAY 151) is pharmacologically inactive and is the hydrolysis product of the cyano moiety, accounting for 57% of the dose, followed by the glucuronide (BQS867) and the amide hydrolysis products (4% of dose). In vitro data in human kidney microsomes suggest that the kidney may be one of the major organs contributing to the hydrolysis of Vildagliptin to its major inactive metabolite, LAY151. DPP-4 contributes partially to the hydrolysis of Vildagliptin based on an in vivo study using DPP-4 deficient rats. Vildagliptin is not metabolised by CYP 450 enzymes to any quantifiable extent. Accordingly, the metabolic clearance of Vildagliptin is not anticipated to be affected by co-medications that are CYP 450 inhibitors and/or inducers. In vitro studies demonstrated that Vildagliptin does not inhibit/induce CYP 450 enzymes. Therefore, Vildagliptin is not likely to affect metabolic clearance of co-medications metabolised by CYP 1A2, CYP 2C8, CYP 2C9, CYP 2C19, CYP 2D6, CYP 2E1 or CYP 3A4/5.
Elimination
Following oral administration of [14C] Vildagliptin, approximately 85% of the dose was excreted into the urine and 15% of the dose is recovered in the faeces. Renal excretion of the unchanged Vildagliptin accounted for 23% of the dose after oral administration. After intravenous administration to healthy subjects, the total plasma and renal clearances of Vildagliptin are 41 and 13 l/h, respectively. The mean elimination half-life after intravenous administration is approximately 2 hours. The elimination half-life after oral administration is approximately 3 hours.
6.0 Nonclinical properties
6.1 Animal toxicology or pharmacology
Intra-cardiac impulse conduction delays were observed in dogs with a no-effect dose of 15 mg/kg (7-fold human exposure based on Cmax). Accumulation of foamy alveolar macrophages in the lung was observed in rats and mice. The noeffect dose in rats was 25 mg/kg (5-fold human exposure based on AUC) and in mice 750 mg/kg (142-fold human exposure). Gastrointestinal symptoms, particularly soft faeces, mucoid faeces, diarrhoea and, at higher doses, faecal blood were observed in dogs. A no-effect level was not established. Vildagliptin was not mutagenic in conventional in vitro and in vivo tests for genotoxicity. A fertility and early embryonic development study in rats revealed no evidence of impaired fertility, reproductive performance or early embryonic development due to Vildagliptin. Embryofoetal toxicity was evaluated in rats and rabbits. An increased incidence of wavy ribs was observed in rats in association with reduced maternal body weight parameters, with a no-effect dose of 75 mg/kg (10-fold human exposure). In rabbits, decreased foetal weight and skeletal variations indicative of developmental delays were noted only in the presence of severe maternal toxicity, with a no-effect dose of 50 mg/kg (9-fold human exposure). A pre- and postnatal development study was performed in rats. Findings were only observed in association with maternal toxicity at ≥ 150 mg/kg and included a transient decrease in body weight and reduced motor activity in the F1 generation.
A two-year carcinogenicity study was conducted in rats at oral doses up to 900 mg/kg (approximately 200 times human exposure at the maximum recommended dose). No increases in tumour incidence attributable to Vildagliptin were observed. Another two-year carcinogenicity study was conducted in mice at oral doses up to 1,000 mg/kg. An increased incidence of mammary adenocarcinomas and haemangiosarcomas was observed with a no-effect dose of 500 mg/kg (59-fold human exposure) and 100 mg/kg (16-fold human exposure), respectively. The increased incidence of these tumours in mice is considered not to represent a significant risk to humans based on the lack of genotoxicity of Vildagliptin and its principal metabolite, the occurrence of tumours only in one species and the high systemic exposure ratios at which tumours were observed.
In a 13-week toxicology study in cynomolgus monkeys, skin lesions have been recorded at doses ≥ 5 mg/kg/day. These were consistently located on the extremities (hands, feet, ears and tail). At 5 mg/kg/day (approximately equivalent to human AUC exposure at the 100 mg dose), only blisters were observed. They were reversible despite continued treatment and were not associated with histopathological abnormalities. Flaking skin, peeling skin, scabs and tail sores with correlating histopathological changes were noted at doses ≥ 20 mg/kg/day (approximately 3 times human AUC exposure at the 100 mg dose). Necrotic lesions of the tail were observed at ≥ 80 mg/kg/day. Skin lesions were not reversible in the monkeys treated at 160 mg/kg/day during a 4-week recovery period.
7.0 Description
Vildagliptin, a member of the islet enhancer class, is a potent and selective DPP-4 inhibitor.
8.0 Pharmaceutical particulars
8.1 Incompatibilities
Not applicable
8.2 Shelf-life
24 Months
8.3 Packaging information
Alu-Alu blister strip of 15 tablets.
8.4 Storage and handing instructions
Store protected from moisture at a temperature not exceeding 30°C.
Keep out of reach of children.
9.0 Patient Counselling Information
- Do not take this medicine, if you are allergic to Vildagliptin.
- Signs of an allergic reaction include a rash, itching or shortness of breath.
- If you get any side effects, talk to your doctor or pharmacist. This includes any possible side effects not listed in this leaflet.
- If you have any further questions, ask your doctor or pharmacist.
12.0 Date of issue
02 March 2022
About leaflet
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor, pharmacist or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
What is in this leaflet
- What VIL G is and what it is used for
- What you need to know before you take VIL G
- How to take VIL G
- Possible side effects
- How to store VIL G
- Contents of the pack and other information
1. What Vil G is and What It is Used for
The active substance of VIL G, vildagliptin, belongs to a group of medicines called “oral antidiabetics”.
VIL G is used to treat adult patients with type 2 diabetes. It is used when diabetes cannot be controlled by diet and exercise alone. It helps to control the level of sugar in the blood. Your doctor will prescribe. VIL G either alone or together with certain other antidiabetic medicines which you will already be taking, if these have not proved sufficiently effective to control diabetes.
Type 2 diabetes develops if the body does not make enough insulin or if the insulin that the body makes does not work as well as it should. It can also develop if the body produces too much glucagon.
Insulin is a substance which helps to lower the level of sugar in the blood, especially after meals. Glucagon is a substance which triggers the production of sugar by the liver, causing the blood sugar level to rise. The pancreas makes both of these substances.
How VIL G works
VIL G works by making the pancreas produce more insulin and less glucagon. This helps to control the blood sugar level. This medicine has been shown to reduce blood sugar, which may help to prevent complications from your diabetes. Even though you are now starting a medicine for your diabetes, it is important that you continue to follow the diet and/or exercise which has been recommended for you.
2. What You Need to Know Before You Take Vil G
Do not use VIL G
if you are allergic to vildagliptin or any of the other ingredients of this medicine. If you think you may be allergic to vildagliptin or any of the other ingredients of, do not take this medicine and talk to your doctor.
Warnings and precautions
Talk to your doctor or pharmacist before using VIL G:
if you have type 1 diabetes (i.e. your body does not produce insulin) or if you have a condition called diabetic ketoacidosis.
if you are taking an anti-diabetic medicine known as a sulphonylurea (your doctor may want to reduce your dose of the sulphonylurea when you take it together with VIL G in order to avoid low blood glucose [hypoglycaemia]).
if you have moderate or severe kidney disease (you will need to take a lower dose of VIL G).
if you are on dialysis.
if you have liver disease.
if you suffer from heart failure.
if you have or have had a disease of the pancreas.
If you have previously taken vildagliptin but had to stop taking it because of liver disease, you should not take this medicine.
Diabetic skin lesions are a common complication of diabetes. You are advised to follow the recommendations for skin and foot care that you are given by your doctor or nurse. You are also advised to pay particular attention to new onset of blisters or ulcers while taking VIL G. Should these occur, you should promptly consult your doctor. A test to determine your liver function will be performed before the start of VIL G treatment, at three month intervals for the first year and periodically thereafter. This is so that signs of increased liver enzymes can be detected as early as possible.
Children and adolescents
The use of VIL G in children and adolescents up to 18 years of age is not recommended.
Other medicines and VIL G
Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines.
Your doctor may wish to alter your dose of VIL G if you are taking other medicines such as:
thiazides or other diuretics (also called water tablets)
corticosteroids (generally used to treat inflammation)
thyroid medicines
certain medicines affecting the nervous system.
Pregnancy and breast-feeding
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine. You should not use VIL G during pregnancy. It is not known if VIL G passes into breast milk. You should not use VIL G if you are breast-feeding or plan to breast-feed.
Driving and using machines
If you feel dizzy while taking VIL G, do not drive or use machines.
3. How to Use Vil G
Always take this medicine exactly as your doctor has told you. Check with your doctor or pharmacist if you are not sure.
How much to take and when
The amount of VIL G people have to take varies depending on their condition. Your doctor will tell you exactly how many tablets of VIL G to take. The maximum daily dose is 100 mg.
The usual dose of VIL G is either:
- 50 mg daily taken as one dose in the morning if you are taking VIL G with another medicine called a sulphonylurea.
- 100 mg daily taken as 50 mg in the morning and 50 mg in the evening if you are taking VIL G alone, with another medicine called metformin or a glitazone, with a combination of metformin and a sulphonylurea, or with insulin.
- 50 mg daily in the morning if you have moderate or severe kidney disease or if you are on dialysis.
How to take VIL G
Swallow the tablets whole with some water.
How long to take VIL G
- Take VIL G every day for as long as your doctor tells you. You may have to take this treatment over a long period of time.
- Your doctor will regularly monitor your condition to check that the treatment is having the desired effect.
If you take more VIL G than you should
If you take too many VIL G tablets, or if someone else has taken your medicine, talk to your doctor straight away. Medical attention may be needed. If you need to see a doctor or go to the hospital, take the pack with you.
If you forget to take VIL G
If you forget to take a dose of this medicine, take it as soon as you remember. Then take your next dose at the usual time. If it is almost time for your next dose, skip the dose you missed. Do not take a double dose to make up for a forgotten tablet.
If you stop taking VIL G
Do not stop taking VIL G unless your doctor tells you to. If you have questions about how long to take this medicine, talk to your doctor.
4. Possible Side Effects
Like all medicines, this medicine can cause side effects, although not everybody gets them.
Some symptoms need immediate medical attention:
You should stop taking VIL G and see your doctor immediately if you experience the following side effects:
- Angioedema (rare: may affect up to 1 in 1,000 people): Symptoms include swollen face, tongue or throat, difficulty swallowing, difficulties breathing, sudden onset rash or hives, which may indicate a reaction called “angioedema”.
- Liver disease (hepatitis) (rare): Symptoms include yellow skin and eyes, nausea, loss of appetite or dark-coloured urine, which may indicate liver disease (hepatitis).
- Inflammation of the pancreas (pancreatitis) (frequency not known): Symptoms include severe and persistent pain in the abdomen (stomach area), which might reach through to your back, as well as nausea and vomiting.
Other side effects
Some patients have had the following side effects while taking VIL G and metformin:
- Common (may affect up to 1 in 10 people): Trembling, headache, dizziness, nausea, low blood glucose
- Uncommon (may affect up to 1 in 100 people): Tiredness
Reporting of side effects
If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. You can also report side effects directly: Website: www.zuventus.com and click the tab “Safety Reporting” located on the top right end of the home page.
By reporting side effects, you can help provide more information on the safety of this medicine. You can also report the side effect with the help of your treating physician.
5. How to Store Vil G
- Store protect from moisture, at a temperature not exceeding 30°C.
- Keep out of reach of children.
- Do not use this medicine after the expiry date which is stated on the blister and the carton after “EXP”. The expiry date refers to the last day of that month.
6. Contents of the Pack and Other Information
What VIL G contains
Each film coated tablet contains
Vildagliptin 50 mg
Excipients q.s.
© Zuventus Healthcare Ltd., 2020. All rights reserved.