Zuviston Tablets
Therapy Area
Women's Health
1.0 Generic name
Dydrogesterone Tablets IP 10 mg
2.0 Qualitative and quantitative composition
Each film coated tablet contains :
Dydrogesterone IP 10 mg
Colour : Titanium Dioxide IP
3.0 Dosage form and strength
Tablet 10 mg
4.0 Clinical particulars
4.1 Therapeutic indication
Progesterone deficiencies
- Treatment of dysmenorrhoea
- Treatment of endometriosis.
- Treatment of secondary amenorrhoea.
- Treatment of irregular cycles.
- Treatment of dysfunctional uterine bleeding.
- Treatment of pre-menstrual syndrome.
- Treatment of threatened abortion.
- Treatment of habitual abortion.
- Treatment of infertility due to luteal insufficiency.
- Luteal Support as a part of Assisted Reproductive Technology (ART) treatment.
Hormone replacement therapy
To counteract the effects of unopposed oestrogen on the endometrium in hormone replacement therapy for women with disorders due to natural or surgical induced menopause with an intact uterus.
4.2 Posology and method of administration
Dosages, treatment schedule and duration of treatment may be adapted to the severity of the dysfunction and the clinical response.
Dysmenorrhoea : 10 or 20 mg Dydrogesterone per day from day 5 to day 25 of the Menstrual cycle.
Dysfunctional uterine bleeding : When treatment is started to arrest a bleeding episode, 20 or 30 mg Dydrogesterone per day is to be given for up to 10 days. For continuous treatment, 10 or 20 mg Dydrogesterone per day should be given during the second half of the menstrual cycle. The starting day and the number of treatment days will depend on the individual cycle length.
Withdrawal bleeding occurs if the endometrium has been adequately primed with either endogenous or exogenous estrogen.
Secondary amenorrhoea : 10 or 20 mg Dydrogesterone per day, to be given daily for 14 days during the second half of the theoretical menstrual cycle to produce an optimum secretory transformation of an endometrium that has been adequately primed with either endogenous or exogenous estrogen.
Pre-menstrual syndrome : 10 mg Dydrogesterone twice daily starting with the secondhalf of the menstrual cycle until the first day of the next cycle. The starting day and the number of treatment days will depend on the individual cycle length.
Irregular cycles : 10 or 20 mg Dydrogesterone per day starting with the second half of the menstrual cycle until the first day of the next cycle. The starting day and the number of treatment days will depend on the individual cycle length.
Threatened abortion : An initial dose of up to 40 mg Dydrogesterone may be given followed by 20 or 30 mg per day until symptoms remit
Habitual abortion : 10 mg Dydrogesterone twice daily until the twentieth week of pregnancy.
Infertility due to luteal insufficiency : 10 or 20 mg Dydrogesterone daily starting with the second half of the menstrual cycle until the first day of the next cycle. Treatment should be maintained for at least three consecutive cycles.
Hormone replacement therapy :
- Continuous sequential therapy : An estrogen is dosed continuously and one tablet of 10 mg Dydrogesterone is added for the last 14 days of every 28 day cycle, in a sequential manner.
- Cyclic therapy : When an estrogen is dosed cyclically with a treatment-free interval, usually 21 days on and 7 days off. One tablet of 10 mg Dydrogesterone is added for the last 12 -14 days of estrogen therapy.
- Depending on the clinical response, the dosage can subsequently be adjusted to 20 mg Dydrogesterone per day.
There is no relevant use of Dydrogesterone before menarche. The safety and efficacy of Dydrogesterone in adolescents aged 12-18 years has not been established. Currently available data are described in 'Adverse Reactions and 'Pharmacodynamic Properties', but no recommendation on a posology can be made.
4.3 Contraindications
- Hypersensitivity to the active substance or to any of the excipients.
- Known or suspected progestogen dependent neoplasms (e.g. meningioma)
- Undiagnosed vaginal bleeding.
- If used to prevent endometrial hyperplasia (in women using estrogens) : Contraindications for use of oestrogens in combination with progestagens, such as Dydrogesterone.
4.4 Special warnings and precautions for use
Before initiating Dydrogesterone treatment for abnormal bleeding the etiology for the bleeding should be clarified. Breakthrough bleeding and spotting may occur during the first months of treatment. If breakthrough bleeding or spotting appears after some time on therapy, or continues after treatment has been discontinued, the reason should be investigated, which may include endometrial biopsy to exclude endometrial malignancy.
Conditions which need supervision
If any of the following conditions are present, have occurred previously, and/or have been aggravated during pregnancy or previous hormone treatment, the patient should be closely supervised. It should be taken into account that these conditions may recur or be aggravated during treatment with Dydrogesterone and ceasing the treatment should be considered :
Porphyria
Depression
Abnormal liver function values caused by acute or chronic liver disease
Other conditions
Patients with rare hereditary problems of galactose intolerance, Lapp lactase deficiency or glucosegalactose malabsorption should not take this medicine.
The following warnings and precautions apply when using Dydrogesterone in combination with estrogens for hormone replacement therapy (HRT) :
See also the warnings and precautions in the product information of the estrogen preparation.
For the treatment of postmenopausal symptoms, HRT should only be initiated for symptoms that adversely affect quality of life. In all cases, a careful appraisal of the risks and benefits should be undertaken at least annually and HRT should only be continued as long as the benefit outweighs the risk. Evidence regarding the risks associated with HRT in the treatment of premature menopause is limited. Due to the low level of absolute risk in younger women, however, the balance of benefits and risks for these women may be more favourable than in older women.
Medical examination / follow-up
Before initiating or reinstituting HRT, a complete personal and family medical history should be taken. Physical (including pelvic and breast) examination should be guided by this and by the contraindications and warnings for use. During treatment, periodic check-ups are recommended of a frequency and nature adapted to the individual woman. Women should be advised what changes in their breasts should be reported to their doctor or nurse (see 'Breast cancer' below). Investigations, including appropriate imaging tools, e.g., mammography, should be carried out in accordance with currently accepted screening practices, modified to the clinical needs of the individual.
Endometrial hyperplasia
Long-term use of oestrogens without addition of progestagens increases the change of endometrial hyperplasia and endometrial carcinoma in women with a uterus. This risk may largely be prevented by combining the oestrogen therapy for at least 12 days per cycle with a progestagen, such as Dydrogesterone.
Breast cancer
The overall evidence suggests an increased risk of breast cancer in women taking combined estrogen-progestogen and possibly also estrogen-only HRT, that is dependent on the duration of taking HRT. The excess risk becomes apparent within a few years of use but returns to baseline within a few (at most five) years after stopping treatment. HRT, especially estrogen-progestogen combined treatment, increases the density of mammographic images which may adversely affect the detection of breast cancer.
Ovarian cancer
Ovarian cancer is much rarer than breast cancer. Epidemiological evidence from a large meta-analysis suggests a slightly increased risk in women taking oestrogen-only or combined oestrogen-progestogen HRT, which becomes apparent within 5 years of use and diminishes over time after stopping. Some other studies including the WHI trial suggest that use of combined HRTs may be associated a similar, or slightly smaller, risk.
Venous thrombo-embolism
HRT is associated with a 1.3-3 fold risk of developing venous thromboembolism (VTE), i.e., deep vein thrombosis or pulmonary embolism. The occurrence of such an event is more likely in the first year of HRT than later. Patients with known thrombophilic states have an increased risk of VTE and HRT may add to this risk. HRT is therefore contraindicated in these patients. Generally recognized risk factors for VTE include, use of estrogens, older age, major surgery, prolonged immobilization, obesity (BMI > 30 kg/m2), pregnancy/ postpartum period, systemic lupus erythematosus (SLE), and cancer. There is no consensus about the possible role of varicose veins in VTE. As in all postoperative patients, prophylactic measures need be considered to prevent VTE following surgery. If prolonged immobilization is to follow elective surgery temporarily stopping HRT 4 to 6 weeks earlier is recommended. Treatment should not be restarted until the woman is completely mobilized. In women with no personal history of VTE but with a first degree relative with a history of thrombosis at young age, screening may be offered after careful counselling regarding its limitations (only a proportion of thrombophilic defects are identified by screening). If a thrombophilic defect is identified which segregates with thrombosis in family members or if the defect is 'severe' (e.g., antithrombin, protein S, or protein C deficiencies or a combination of defects) HRT is contraindicated. Women already on chronic anticoagulant treatment require careful consideration of the benefit risk of use of HRT. If VTE develops after initiating therapy, the drug should be discontinued. Patients should be told to contact their doctors immediately when they are aware of a potential thromboembolic symptom (e.g. painful swelling of a leg, sudden pain in the chest, dyspnea).
Coronary artery disease (CAD)
There is no evidence from randomized controlled trials of protection against myocardial infarction in women with or without existing CAD who received combined estrogenprogestogen or estrogen-only HRT
Combined estrogen-progestogen therapy
The relative risk of CAD during use of combined estrogen progestogen HRT is slightly increased. As the baseline absolute risk of CAD is strongly dependent on age, the number of extra cases of CAD due to estrogen-progestogen use is very low in healthy women close to menopause, but will rise with more advanced age.
Cerebrovascular accident (CVA)
Combined estrogen-progestogen and estrogen-only therapy are associated with an up to 1.5-fold increase in risk of ischemic stroke. The relative risk does not change with age or time since menopause. However, as the baseline risk of stroke is strongly agedependent, the overall risk of stroke in women who use HRT will increase with age.
4.5 Drugs interactions
In vitro data show that the major metabolic pathway generating the main pharmacologically active metabolite 20α Dihydrodydrogesterone (DHD) is catalyzed by aldo-keto reductase 1C (AKR 1C) in human cytosol. Next to the cytosolic metabolism there are metabolic transformations by cytochrome P450 iso-enzymes (CYPs), nearly exclusively via CYP3A4, resulting in several minor metabolites. The main active metabolite DHD is substrate for metabolic transformation by CYP3A4. Therefore, the metabolism of Dydrogesterone and DHD may be increased by concomitant use of substances known to induce CYP enzymes such as anticonvulsants (e.g., Phenobarbital, Phenytoin, Carbamazepine), anti-infectives (e.g., Rifampicin, Rifabutin, Nevirapine, Efavirenz) and herbal preparations containing e.g. St John's Wort (Hypericumperforatum), sage, or gingko biloba. Ritonavir and nelfinavir, although known as strong cytochrome enzyme inhibitors, by contrast exhibit enzyme-inducing properties when used concomitantly with steroid hormones. Clinically, an increased metabolism of Dydrogesterone may lead to a decreased effect. In vitro studies have shown that Dydrogesterone and DHD do not inhibit or induce CYP drug metabolizing enzymes at clinically relevant concentrations.
4.6 Use in special populations
Pregnancy
It is estimated that more than 9 million pregnancies have been exposed to Dydrogesterone. So far there were no indications of a harmful effect of Dydrogesterone use during pregnancy. Some progestogens have been reported in the literature to be associated with an increased risk of hypospadias. However due to confounding factors during pregnancy, no definitive conclusion can be drawn regarding the contribution of progestogens to hypospadias. Clinical studies, where a limited number of women were treated with Dydrogesterone early in pregnancy, have not shown any increase in risk. No other epidemiological data are hitherto available. Effects in non-clinical embryo-fetal and post-natal development studies were in line with the pharmacological profile. Untoward effects occurred only at exposures which exceeded the maximum human exposure considerably, indicating little relevance to clinical use. Dydrogesterone can be used during pregnancy if clearly indicated.
Breast feeding
No data exist on excretion of Dydrogesterone in mother's milk. Experience with other progestogens indicates that progestogens and the metabolites pass to mother's milk in small quantities. Whether there is a risk to the child is not known. Therefore, Dydrogesterone should not be used during the lactation period.
Fertility
There is no evidence that Dydrogesterone decreases fertility at therapeutic dose.
4.7 Effects on ability to drive and use machines
Dydrogesterone has a slight effect on ability to drive and to use machinery. In rare cases Dydrogesterone may cause somnolence and/or dizziness, in particular during the first couple of hours after taking it. Caution is therefore advised when driving and operating machinery.
4.8 Undesirable effects
| Organ class according to MedDRA database | Common ≥1:100, <1:10 | Uncommon ≥1:1,000, <1:100 | Rare ≥1:10,000, <1:1,000 |
| Neoplasms, benign, Malignant and nonspecified (including cysts and polyps) | Growth of progestogendepen dent neoplasms (e.g. Eningioma)* | ||
| Blood and lymphatic system disorders | Haemolytic anaemia* | ||
| Psychiatric disorders | Depression | ||
| Immune system disorders | Hypersensitivity | ||
| Nervous system disorders | Migraine / Headache | Dizziness | Somnolence |
| Gastrointestinal disorders | Nausea | Vomiting | |
| Hepatobiliary disorders | Disturbed liver function (with Icterus, Asthenia or Malaise, and abdominal pain | ||
| Skin and subcutaneous tissue disorders pruritus, Urticaria) | Allergic dermatitis (e.g. rash, | Angiooedema* | |
| Reproductive system and breast disorders | Disturbed menstruation (including Metrorrhagia, menorrhagia, Oligo- /amenorrhoea, Dysmenorrhoea and Irregular menstruation) Painful/ sensitive breasts | Swelling of the breasts | |
| General disorders and administration site conditions | Oedema | ||
| Investigations | Weight gain |
* Adverse effects reported spontaneously
Undesirable effects that are associated with an estrogen-progestogen treatment (see also 'Warnings and Precautions' and the product information of the estrogen preparation) :
Breast cancer, Endometrial hyperplasia, Endometrial carcinoma, Ovarian cancer
Venous thromboembolism
Myocardial infarction, Coronary artery disease, Ischemic stroke
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via e-mail to : medico@zuventus.com
Website : https://www.zuventus.com/drug-safety-reporting By reporting side effects, you can help provide more information on the safety of this medicine.
4.9 Overdose
Symptoms
Dydrogesterone is a substance with very low toxicity. Nausea, vomiting, lethargy and dizziness are symptoms which may theoretically occur in the event of an overdose. There are no known cases in which an overdose of Dydrogesterone led to harmful effects.
Treatment
Specific treatment is clearly not necessary. In case of overdose symptomatic treatment may be considered.
5.0 Pharmacological properties
5.1 Mechanism of action
Dydrogesterone is an orally-active progestogen which produces a complete secretory endometrium in an estrogen-primed uterus thereby providing protection against the increased risk for endometrium hyperplasia and/or carcinogenesis induced by estrogens. It is indicated in all cases of endogenous progesterone deficiency.
5.2 Pharmacodynamic properties
Dydrogesterone has no estrogenic, no androgenic, no thermogenic, no anabolic and no corticoid activity. Dydrogesterone does not suppress ovulation.
5.3 Pharmacokinetic properties
Absorption
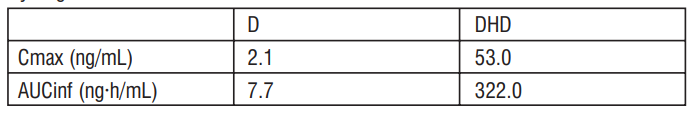
After oral administration Dydrogesterone is rapidly absorbed with a Tmax of between 0.5 and 2.5 hours. The absolute biological availability of Dydrogesterone (20 mg oral dose versus 7.8 mg intravenous infusion) is 28%. The following tables gives the pharmacokinetic parameters of Dydrogesterone (D) and 20α Dihydrodydrogesterone (DHD) after administration of a single dose of 10 mg Dydrogesterone :
Distribution
After intravenous administration of Dydrogesterone the steady-state distribution volume is around 1400 l. More than 90% of Dydrogesterone and DHD are bound to plasma-proteins.
Metabolism
After oral administration Dydrogesterone is quickly metabolised to DHD. The plasma levels of the main active metabolite DHD show a peak around 1.5 hours after administering the dose. The plasma levels of DHD are substantially higher than the related medicinal product. The AUC and Cmax ratios of DHD and Dydrogesterone are of the order of magnitude of respectively 40 and 25. The mean terminal half-life of Dydrogesterone and DHD varies from respectively 5 to 7 and 14 to 17 hours. A common characteristic of all characterised metabolites is the retention of the 4,6-diene-2-one configuration of the original product and the absence of 17α hydroxylation. This explains the absence of oestrogenic and androgenic effects of Dydrogesterone.
Elimination
After oral administration of labelled Dydrogesterone on average 63% of the dose is excreted in the urine. The total plasma clearance is 6.4 l/minute. Within 72 hours the excretion is complete, DHD is present in the urine mainly as the conjugated glucuronic acid.
6.0 Nonclinical properties
6.1 Animal toxicology or pharmacology
Non-clinical data obtained during conventional investigation into the toxixcity of single and repeated doses, genotoxicity and the carcinogenic potential do not show any special risks for humans. Research into the toxic effects on the reproduction of rats shows for high doses (> 80 times the human exposure) an increased incidence of erect nipples (during days 11-19 of the lactation period) and of hypospadia in male rats. The clinical relevance of these observations is not known. The limited data on safety in animals indicate that Dydrogesterone has an extending effect on delivery, which corresponds with the progestogenic action.
7.0 Description
Dydrogesterone is a synthetic progesterone with an oral biological availability that causes a secretory phase of the endometrium in a uterus prepared by oestrogen. It gives protection against the increased risk of endometrial hyperplasia and/or endometrial carcinoma that is induced by oestrogens.
8.0 Pharmaceutical particulars
8.1 Incompatibilities
Not applicable
8.2 Shelf-life
Refer on the pack.
8.3 Packaging information
PVC/PVDC-Alu blister pack of 10 tablets.
8.4 Storage and handing instructions
Store at temperature not exceeding 25°C. Protect from light
Keep out of reach of children.
9.0 Patient counselling information
Ask the patient to report any adverse events.
Ask the patients if Porphyria, Depression, Abnormal liver function values caused by acute or chronic liver disease is present, have occurred previously, and/or have been aggravated during pregnancy or previous hormone treatment.
Patients should be asked to exercise caution when driving and operating machinery
Ask the patient to report if breakthrough bleeding or spotting appears after some time on therapy, or continues after treatment has been discontinued.
12.0 Date of revision
31 May 2022
About leaflet
Read all of this leaflet carefully before you start taking this medicine because it contains important information for you.
- Keep this leaflet. You may need to read it again.
- If you have any further questions, ask your doctor, pharmacist or nurse.
- This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours.
- If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any side effects not listed in this leaflet. See section 4.
What is in this leaflet:
- What Zuviston is and what it is used for
- What you need to know before you take Zuviston
- How to take Zuviston
- Possible side effects
- How to store Zuviston
- Contents of the pack and other information
1. What Zuviston is and what it is used for
What Zuviston is
Zuviston contains a medicine called “dydrogesterone”. Dydrogesterone is a man-made hormone. It is very similar to the hormone “progesterone” made by your body. Medicines like Zuviston are called “progestogens”
What Zuviston is used for
Zuviston can be used alone or with an estrogen. Whether you take an estrogen as well, depends on what you are taking the medicine for.
Zuviston is used:
For problems you may get when your body does not produce enough progesterone:
to relieve painful periods
to relieve the symptoms of endometriosis (a problem caused by growth of the womb lining outside the womb)
to treat infertility due to low level of progesterone to control irregular periods (that come at the wrong time or not at all)
to relieve the symptoms of premenstrual syndrome (PMS).
to re-start periods that have stopped before the menopause (amenorrhoea)
to stop or prevent unusually heavy or long periods (often due to the start of the menopause).
To treat the signs of your menopause – this treatment is called Hormone Replacement Therapy or ‘HRT’.
Zuviston is used with an estrogen to treat the signs of your menopause. These signs vary from woman to woman.
How Zuviston works
Zuviston is used to treat problems which you may get when your body is not making enough of its own progestogen hormone. This is normally produced in your ovaries from puberty until your menopause. The progestogen (dydrogesterone) in Zuviston replaces this missing hormone. In your body, progestogen is normally balanced against the major female hormone estrogen. Your doctor may also have prescribed an estrogen medicine for you so that you get the right balance of hormones. For some women using HRT, taking only an estrogen can cause an abnormal thickening of the womb lining. This may also be the case if you do not have your womb and have a history of endometriosis. Taking dydrogesterone for part of your monthly cycle helps to prevent a build-up of your womb lining.
2. What you need to know before you take Zuviston
If you are just taking Zuviston
Before taking your medicine, you should make sure it is safe for you to do so.
Do not take Zuviston if:
- you have a tumour that is made worse by progestogens (such as meningioma)
- you have irregular or unusually heavy periods that your doctor does not already know about
- you are allergic (hypersensitive) to any of the ingredients of this medicine listed in Section 6
Do not take Zuviston if any of the above apply to you. If you are not sure, talk to your doctor or pharmacist before taking Zuviston.
If you are taking Zuviston together with an estrogen for example part of a HRT, please also read the “Do not take” section on the information leaflet that comes with your estrogen medicine.
Before taking your medicine you should also make sure that it is safe for you to take the estrogen product at the same time.
Warnings and Precautions
If you need to take Zuviston for abnormal bleeding, your doctor will find the cause of the bleeding before you start taking this medicine.
If you get unexpected vaginal bleeding or spotting it is usually nothing to worry about. It is especially likely during the first months of taking Zuviston. However, make an appointment to see your doctor straight away if bleeding or spotting:
- carries on for more than a few months
- starts after you have been on treatment for a while
- carries on even after you have stopped treatment
This may be a sign that your womb lining has become thicker. Your doctor will look into the cause of the bleeding or spotting and may do a test to find out if you have cancer of the womb lining.
Check with your doctor or pharmacist before taking Zuviston if you have any of the following:
- depression
- liver problems
- a rare blood problem passed down in families (inherited) called “porphyria”.
If any of the above apply to you (or you are not sure), talk to your doctor or pharmacist before taking Zuviston. It is particularly important to tell them if the problems above have ever got worse during pregnancy or previous hormone therapy. Your doctor may want to monitor you more closely during treatment. If they get worse or reappear while taking Zuviston, your doctor may stop treatment.
Zuviston and HRT
As well as benefits, HRT has some risks which you and your doctor need to consider when you are deciding whether to take these medicines. If you are taking Zuviston with an estrogen as part of HRT, the following information is important. Please also read the information leaflet that comes with your estrogen medicine.
Early menopause
There is limited evidence about the risks of HRT when it is used to treat early menopause. There is a low level of risk in younger women. This means that the balance of benefits and risks for younger women using HRT for early menopause may be better than in older women.
Medical check-ups
Before you start taking HRT, your doctor should ask about you and your family’s medical history. Your doctor may decide to examine your breasts or your tummy (abdomen) and may do an internal examination.
They will only do this if it is necessary for you or if you have any special concerns.
Once you have started on HRT, see your doctor for regular check-ups (at least once a year), he may do screening tests such as a mammogram (an X-ray of the breasts). At these check-ups, your doctor may discuss the benefits and risks of continuing to take HRT. Make sure that you:
- go for regular breast screening and cervical smear tests
- regularly check your breasts for any changes such as dimpling of the skin, changes in the nipple or any lumps you can see or feel.
Heart disease
HRT will not help to prevent heart disease. HRT is not recommended for women who have heart disease or have had heart disease recently.
The risk of heart disease also increases with age. The number of extra cases of heart disease due to use of estrogenprogestogen HRT is very low in healthy women close to menopause. The number of extra cases increases with age. If you have ever had heart disease, talk to your doctor to see if you should take HRT.
If you get a pain in your chest that spreads to your arm or neck:
- see a doctor as soon as possible
- do not take any more HRT until your doctor says you can.
This pain could be a sign of heart disease.
Stroke
Taking estrogen-progesterone HRT and estrogen only HRT increases the risk of having a stroke. The risk is up to one and a half times that of people not taking HRT. The comparable risk for users, versus non-users, does not change with age or time since menopause. The risk of stroke increases with age.
This means that the general risk of stroke in women who use HRT will increase with age.
If you get an unexplained headache or migraine (which can include disturbed vision):
- see a doctor as soon as possible
- do not take any more HRT until your doctor says you can.
This may be an early warning sign of a stroke.
Blood clots
HRT increases the risk of blood clots in the veins (a deep vein thrombosis or DVT) the risk is up to 3 times higher than that of people not taking HRT, especially during the first year of taking it.
You are more likely to get a blood clot if:
- you are older - you have cancer
- you are very overweight - you are taking an estrogen
- you are pregnant or have recently had a baby
- you (or close family) have had a blood clot before, including in the leg or lung
- you have been off your feet for a long time because of major surgery, injury or illness (see information under “Operations”)
- you have systemic lupus erythematosus (SLE). This is a problem that causes joint pain, skin rashes and fever.
If any of these things apply to you, talk to your doctor to see if you should take HRT.
If you get painful swelling in your leg, sudden chest pain or have difficulty breathing:
- see a doctor as soon as possible
- do not take any more HRT until your doctor says you can.
These may be signs of a blood clot.
Also, tell your doctor or pharmacist if you are taking medicines to prevent blood clots (anti-coagulants) - such as warfarin. Your doctor will pay special attention to the benefits and risks of you taking HRT.
Breast cancer
Women who take estrogen-progestogen HRT or estrogen-only HRT have a higher risk of breast cancer. The risk depends on how long you take HRT. The extra risk of breast cancer goes up the longer you take it, after about 3 (1-4) years. After stopping HRT the extra risk will decrease with time, but the risk may persist for 10 years or more if you have used HRT for more than 5 years. If you notice any changes in your breast, such as:
- dimpling of the skin
- changes in the nipple
- any lumps you can see or feel.
Make an appointment to see your doctor as soon as possible.
Endometrial cancer (cancer of the lining of the womb) and endometrial hyperplasia
Women who have womb and take estrogen-only HRT for a long time have a higher risk of cancer of the lining of the womb (the endometrium) and endometrial hyperplasia (abnormal thickening of the womb lining). Taking Zuviston as well as an estrogen (for at least 12 days per month - or 28 day cycle) or as continuous combined estrogen-progestogen therapy can prevent this extra risk.
Ovarian cancer
Ovarian cancer is rare – much rarer than breast cancer. The use of estrogen-only or combined estrogen-progestogen HRT has been associated with a slightly increased risk of ovarian cancer. The risk of ovarian cancer varies with age. For example, in women aged 50 to 54 who are not taking HRT, about 2 women in 2000 will be diagnosed with ovarian cancer over a 5-year period. For women who have been taking HRT for 5 years, there will be about 3 cases per 2000 users (i.e. about 1 extra case).
Other medicines and Zuviston
Other medicines and Zuviston Please tell your doctor or pharmacist if you are taking or have recently taken any other medicines. This includes medicines obtained without a prescription or herbal medicines. In particular, tell your doctor or pharmacist if you are taking any of the following: These medicines may lower the effect of Zuviston and lead to bleeding or spotting
- medicines for fits (epilepsy) such as phenobarbital, phenytoin or carbamazepine
- medicines for infection such as rifampicin, rifabutin, nevirapine, efavirenz - medicines for HIV infection (AIDS) such as ritonavir or nelfinavir
- herbal medicines containing St John’s Wort (Hypericum perforatum), sage, or ginkgo biloba
If any of the above apply to you (or you are not sure), talk to your doctor or pharmacist before taking Zuviston.
Operations or tests
Tell your doctor if you are going to have surgery. Do this well before the operation. You may need to stop taking HRT about 4 to 6 weeks before the operation to reduce the risk of a blood clot. Your doctor will tell you when you can start taking HRT again. - If you visit a hospital or your family doctor for a blood or urine test, tell them that you are taking Zuviston. This is because this medicine may affect the results of these tests.
Children and young people
Zuviston is not for use in children before their first menstrual bleed. It is not known how safe or effective Zuviston is in young people aged 12-18 years.
Fertility, Pregnancy and breast-feeding
Fertility
There is no evidence that dydrogesterone decreases your fertility, if taken as recommended by your doctor.
Pregnancy
There may be an increased risk of hypospadias (a birth defect of the penis involving the urinary opening) in children whose mothers have taken certain progestogens. However, this increased risk is not yet certain. So far, there is no evidence that taking dydrogesterone during pregnancy is harmful. More than 10 million pregnant women have taken Zuviston.
- Talk to your doctor before taking Zuviston if you are pregnant.
- If you become pregnant or think you might be pregnant see your doctor. Your doctor will discuss with you the benefits and risks of taking Zuviston while you are pregnant.
Breast-feeding
Do not take Zuviston if you are breast-feeding. It is not known if Zuviston passes into mother’s milk and affects the child. Studies of other progestogens show small amounts pass into the mother’s milk.
Driving and using machines
You may feel slightly sleepy or dizzy after taking Zuviston. This is more likely in the first few hours after taking it. If this happens, do not drive or use any tools or machines. Wait to see how Zuviston affects you, before you drive or use any tools or machines.
Zuviston contains milk sugar (lactose). If you have been told by your doctor that you cannot tolerate or digest some sugars (have an intolerance to some sugars), talk to your doctor before taking this medicine.
This includes rare problems passed down in families that affect how the body uses lactose, such as “total lactase deficiency” or “glucose-galactose malabsorption”.
3. How to take Zuviston
Always take Zuviston exactly as your doctor has told you. You should check with your doctor or pharmacist if you are not sure. Your doctor will adjust the dose to suit you. While you are taking Zuviston, you should see your doctor regularly (at least once a year). Your doctor may wish to carry out medical checks, including breast examinations.
Taking this medicine
- Swallow the tablet with water
- You can take your tablet with or without food.
- If you have to take more than one tablet, spread them evenly over the day. For example, take one tablet in the morning and one in the evening.
- Try to take your tablet at the same time each day. This will make sure that there is a constant amount of the medicine in your body. This will also help you remember to take your tablets.
- The score line on each tablet is only to help break the tablets so they are easier to swallow. It should not be used in order to take half a tablet.
How much to take
The number of tablets you take and the days you take them on will depend on what you are being treated for. Your doctor will decide the best time for you to take Zuviston. If you are still having natural periods, day 1 of your cycle is when you start bleeding. If you are not having natural periods, your doctor will decide with you when to start day 1 of the cycle and when to start taking your tablets.
To relieve the symptoms of pre-menstrual syndrome
- Take 2 tablets a day.
- Do this from the second half of your cycle until the first day of your next cycle.
- The starting day and number of days you take your tablets for will depend on the length of your cycle.
- Your doctor may decide to give you a higher dose.
To relieve the symptoms of endometriosis
- Take 2 to 3 tablets a day.
- You will either be asked to take your tablets:
- On every day of your cycle or
- only on cycle days 5 to 25.
To treat infertility due to low levels of progesterone
- Take 2 tablets a day.
- Do this from the second half of your cycle until the first day of your next cycle.
- The starting day and number of days you take your tablets for will depend on the length of your cycle.
- Continue treatment for at least three cycles in a row.
- If you become pregnant, tell your doctor.
For irregular periods
- Take 2 tablets a day.
- Do this from the second half of your cycle until the first day of your next cycle.
- The starting day and number of days you take your tablets for will depend on the length of your cycle.
To re-start periods that have stopped before the menopause
- Take 2 tablets a day.
- Do this for fourteen days during the second half of your expected cycle.
For menstrual bleeding that is unusually heavy or happens between periods
- When treatment is started to stop bleeding:
-Take 2 tablets a day
-Do this for five to seven days.
- For continuous treatment:
-Take 2 tablets a day
-Do this during the second half of your cycle.
- The starting day and number of days you take your tablets for will depend on the length of your cycle.
To relieve painful periods
- Cycle days 5 to 25: Take 2 tablets a day.
For hormone replacement therapy (HRT)
- If you are on ‘sequential’ HRT (you take an estrogen tablet or use a patch for your whole cycle):
-Take 1 tablet a day
-Do this for the last fourteen days of the estrogen therapy.
Children and young people
Zuviston is not for use in children before their first menstrual bleed. It is not known how safe or effective Zuviston is in young people aged 12-18 years.
Older people (over 65)
You can use this medicine for HRT. Follow the instructions above for adults.
If you take more Zuviston than you should
If you (or someone else or a child) take too many Zuviston tablets, they are unlikely to do any harm. No treatment is necessary. You may feel sick (nauseous), sleepy, dizzy or be sick (vomit). If you are worried, talk to your doctor for advice.
If you forget to take Zuviston
- If you forget to take today’s tablet and it is less than 12 hours late, take it as soon as you remember. Take the next day’s tablet at the normal time.
- If it is more than 12 hours since you should have taken your tablet, miss this tablet out. Take the next day’s tablet at the usual time and continue taking your tablets as normal.
- Do not take a double dose to make up for a forgotten dose.
- If you miss a tablet, it is more likely that you will have irregular bleeds or spotting.
If you stop taking Zuviston
Do not stop taking Zuviston without talking to your doctor first.
4. Possible side effects
Like all medicines, Zuviston can cause side effects, although not everybody gets them. The following side effects may happen with this medicine.
Side effects of taking Zuviston alone
Stop taking Zuviston and see a doctor straight away or go to hospital, if you notice or suspect any of the following. You may need urgent medical treatment: -
swelling of the skin around the face and throat which may cause difficulty breathing (angioedema)
– affect less than 1 in 1,000 people).
- liver problems
– the signs may include yellowing of the skin or eyes (jaundice), feeling generally unwell with abdominal pain or other liver related changes
– affect less than 1 in 100 people.
- allergic reactions
- the signs may include difficulty breathing or reactions involving the whole body such as feeling sick, being sick, diarrhoea or low blood pressure (affects less than 1 in 1,000 people)
If you notice or suspect any of the above, stop taking Zuviston and see a doctor straight away.
Other side effects of taking Zuviston alone:
Common (affects less than 1 in 10 people)
- headache,
- migraine
- feeling sick (nausea)
- breast pain/tender breasts
- painful, heavy or irregular periods
- no periods or periods happening less often than normal
Uncommon (affects less than 1 in 100 people)
- weight gain
- rash, severe itching or hives
- feeling depressed
- feeling dizzy
- being sick (vomiting)
Rare (affects less than 1 in 1,000 people)
- low levels of red blood cells (haemolytic anaemia)
- hypersensitivity reactions
- your body holding onto more water than usual (fluid retention)
- swelling of the breasts
- feeling sleepy
- increase in the size of tumours affected by progestogens (such as meningioma)
- worsening of a rare blood pigment disorder (porphyria).
Side effects in younger patients are expected to be similar to those seen in adults.
Side effects of taking Zuviston with an estradiol (estrogen-progestogen HRT)
If you are taking Zuviston together with an estrogen please also read the information leaflet that comes with your estrogen medicine. See Section 2 “Before you take Zuviston” for more information on the side effects below.
Stop taking Zuviston and see a doctor straight away, if you notice any of the following side effects:
- painful swelling in your leg, sudden chest pain or difficulty breathing. These could be signs of a blood clot
- pain in your chest that spreads to your arm or neck. This could be a sign of a heart attack
- severe, unexplained headache or migraine (with or without vision problems). These could be signs of a stroke. Stop taking Zuviston and see a doctor straight away, if you notice any of the side effects above.
Make an appointment to see a doctor straight away if you notice:
- dimpling of the skin in your breast, changes in the nipple or lumps you can see or feel. These could be signs of breast cancer. Other side effects of taking Zuviston with an estrogen include abnormal thickening or cancer of the lining of the womb and ovarian cancer.
Reporting of side effects
If you get any side effects, talk to your doctor. This includes any possible side effects not listed in this leaflet. You can also report side effects directly: Website: www.zuventus.com and click the tab “Safety Reporting” located on the top right end of the home page. By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store Zuviston
Keep out of the reach and sight of children. Do not take the tablets after the expiry date shown on the outer carton and blister strip. The expiry date refers to the last day of that month. Do not throw away any medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help protect the environment. This medicinal product does not require any special storage condition
Contents of the pack and other information
What Zuviston contains
The active substance is dydrogesterone.
Each film coated tablet contains:
Dydrogesterone IP 10 mg
Excipients q.s.
Colour Titanium Dioxide IP
Zuviston is available in blister packing.
One blister strip contains 10 tablets.
Marketing Authorisation Holder
Zuventus Healthcare Limited
Zuventus House, Plot Y2, CTS No.: 358/A2,
Near Nahur Railway Station,
Nahur (W), Mumbai, 400078 Maharashtra, India.