The journey towards reaping the benefits of probiotics begins with the right strains and formulations. Selecting the right probiotic tailored to your specific needs can make a significant difference in achieving optimal gut health and overall well-being. Gut Matters!!
Probiotics positively influence gut health by restoring or maintaining a healthy balance of beneficial microorganisms in the gut.
Any Probiotic is successful only when it is effective and have defined results.
De Simone Probiotic is a clinically proven therapy and is recognised in important health guidelines for its efficacy and benefits.
Uniqueness and Originality of strains is most crucial in any Probiotic Formulation
De Simone Formulation contains 8 LIVE bacteria strains (112.5 Bn CFU).
Backed by over 60 trials and 200 publications, DSF is a drug category probiotic and not a food license product
Low FODMAP diet improves symptoms of IBS
But this could be at the cost of Intestinal Flora
The need is to provide protective benefits of De Simone Formulation of Probiotics
De Simone Probiotic in India is Florimax
Among IBS patients, those with visceral hypersensitivity show a specific fungal signature.
There is a need of a Unique & Original Probiotic like De Simone Formulation, which in India is, Florimax
Gut Dysbiosis is a common problem which needs a proven solution. A drug category, unique, multi-strain, high potency original De Simone Probiotic which has been tested in rigorous clinical trials is a promising approach.
GUT MATTERS!!!
Gut imbalance can lead to inflammation, compromised immune function and metabolic disturbances.
The De Simone Formulation Probiotic has been proven effective with backup studies in combating these diseases
Gut Matters!!
Gutflora – Florimax
Dysbiosis can lead to many chronic diseases of gut and more.
A drug category, unique multi-strain, high potency original de simone probiotic, endorsed by international guidelines is the need of the hour.
However,low FODMAP diet is known to cause Bifidobacteria depletion.
Hence,Probiotics containing Bifidobacteria are recommended in IBS patients on low FODMAP diet.
De Simone Probiotic is a Unique & Original blend of Bifidobacteria,Lactobacilli strains.
Original De Simone Probiotic,in India,is Florimax
C Tax-O 200 Tablets
1.0 Generic name
Cefixime Dispersible Tablets IP 100 mg
Cefixime Tablets IP
2.0 Qualitative and quantitative composition
C Tax-O 100 DT
Each uncoated dispersible tablet contains:
Cefixime IP (as Trihydrate) equivalent to
Cefixime (Anhydrous)………………………… 100 mg
Excipients………………………………………...q.s.
Colour: Lake of Quinoline Yellow
Flavour added
C Tax-O 200
Each film coated tablet contains:
Cefixime IP (as Trihydrate)
equivalent to Cefixime (Anhydrous) ………………………200 mg
Excipients…………………………………… q.s.
Colour: Titanium Dioxide IP
3.0 Dosage form and strength
100mg uncoated dispersible Tablets
200mg Tablets
4.0 Clinical particulars
4.1.Therapeutic indications
Oral cephalosporin- in the treatment of
- Urinary tract infection (UTI)
- Respiratory tract infections: upper respiratory tract infections (URTI) and lower respiratory tract infections
- Biliary tract infections
4.2. Posology and method of administration
The usual course of treatment is 7 days. This may be continued for up to 14 days if required.
Posology
Adults and Children over 10 years or weighing more than 50 kg:
The recommended dose is 200 – 400 mg daily according to the severity of infection, given either as a single dose or in two divided doses.
Elderly: Elderly patients may be given the same dose as recommended for adults. Renal function should be assessed and dosage should be adjusted in severe renal impairment.
Pediatric Patients (6 months or older)
The recommended dose is 8 mg/kg/day of the suspension. This may be administered as a single daily dose or may be given in two divided doses, as 4 mg/kg every 12 hours.
Table 1. Suggested doses for pediatric patients
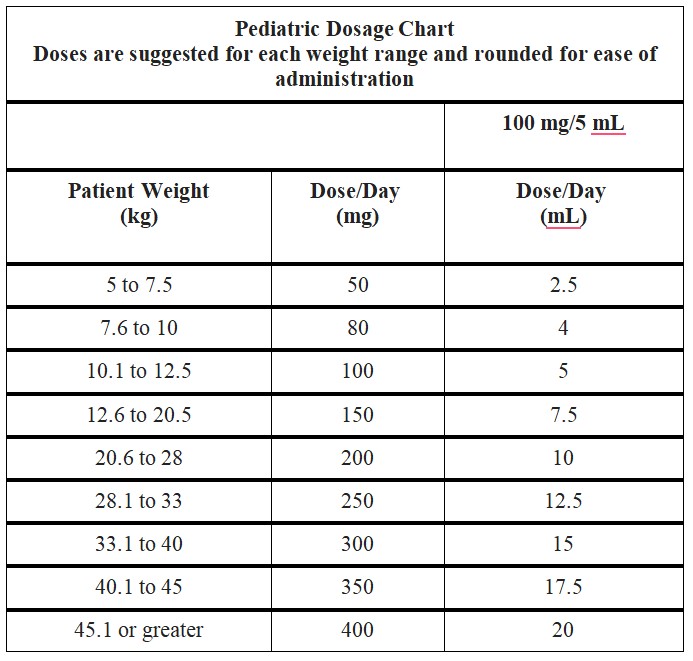
Safety and effectiveness of cefixime in children aged less than six months old have not been established.
Children weighing more than 45 kg or older than 12 years should be treated with the recommended adult dose.
In the treatment of infections due to Streptococcus pyogenes, a therapeutic dosage of cefixime should be administered for at least 10 days.
Renal impairment:
| Creatinine Clearance (mL/min) | 100 mg/5 mL | 200 mg Tablet |
| 20 ml/min or greater. | Normal dose | Normal dose |
| 20 or less OR continuous peritoneal dialysis | 8.6 ml | 200 mg once daily should not be exceeded |
Method for administration:
4.3.Contraindications
Hypersensitivity to cephalosporin antibiotics or to any of the excipients.
4.4. Special warnings and precautions for use
Encephalopathy
Beta-lactams, including cefixime, predispose the patient to encephalopathy risk (which may include convulsions, confusion, impairment of consciousness, movement disorders), particularly in case of overdose or renal impairment.
Severe cutaneous adverse reactions
Severe cutaneous adverse reactions (SCARS) including toxic epidermal necrolysis (TEN), Stevens-Johnson syndrome (SJS) drug rash with eosinophilia and systemic symptoms (DRESS), and acute generalised exanthematous pustulosis (AGEP) have been reported in association with cefixime. Patients should be informed about the signs and symptoms of serious skin manifestations and monitored closely. Treatment should be discontinued at the first appearance of skin rash, mucosal lesions, or any other sign of skin hypersensitivity.
Cefixime should be given with caution to patients who have shown hypersensitivity to other drugs.
Hypersensitivity to penicillins
As with other cephalosporins, cefixime should be given with caution to patients with a history of hypersensitivity to penicillin, as there is some evidence of partial cross-allergenicity between the penicillins and cephalosporins.
Patients have had severe reactions (including anaphylaxis) to both classes of drugs. If an allergic effect occurs with Cefixime, the drug should be discontinued and the patient treated with appropriate agents if necessary.
Haemolytic anaemia
Drug-induced haemolytic anaemia, including severe cases with a fatal outcome, has been described for cephalosporins (as a class). The recurrence of haemolytic anaemia after re-administration of cephalosporins in a patient with a history of cephalosporin (including cefixime) – associated haemolytic anaemia has also been reported.
Acute renal failure
As with other cephalosporins, cefixime may cause acute renal failure including tubulointerstitial nephritis as an underlying pathological condition. When acute renal failure occurs, cefixime should be discontinued and appropriate therapy and/or measures should be taken.
Renal impairment
Cefixime should be administered with caution in patients with markedly impaired renal function.
Paediatric use
Safety of cefixime in premature or new-born infant has not been established.
Antibiotic-associated colitis
Treatment with broad spectrum antibiotics alters the normal flora of the colon and may permit overgrowth of clostridia. Studies indicate that a toxin produced by Clostridium difficile is a primary cause of antibiotic-associated diarrhoea. Pseudomembranous colitis is associated with the use of broad-spectrum antibiotics (including macrolides, semi-synthetic penicillins, lincosamides and cephalosporins); it is therefore important to consider its diagnosis in patients who develop diarrhoea in association with the use of antibiotics. Symptoms of pseudomembranous colitis may occur during or after antibiotic treatment. Management of pseudomembranous colitis should include sigmoidoscopy, appropriate bacteriologic studies, fluids, electrolytes and protein supplementation. If the colitis does not improve after the drug has been discontinued, or if the symptoms are severe, oral vancomycin is the drug of choice for antibiotic-associated pseudomembranous colitis produced by C. difficile. Other causes of colitis should be excluded.
4.5. Interaction with other medicinal products and other forms of interaction
Anticoagulants
In common with other cephalosporins, increases in prothrombin times have been noted in a few patients. Care should therefore be taken in patients receiving anticoagulation therapy.
Cefixime should be administered with caution to patients receiving coumarin-type anticoagulants, e.g. warfarin potassium. Since cefixime may enhance effects of the anticoagulants, prolonged prothrombin time with or without bleeding may occur.
Other forms of interaction
A false positive reaction for glucose in the urine may occur with Benedict's or Fehling's solutions or with copper sulphate test tablets, but not with tests based on enzymatic glucose oxidase reactions.
A false positive direct Coombs test has been reported during treatment with cephalosporin antibiotics, therefore it should be recognised that a positive Coombs test may be due to the drug.
4.6. Fertility, pregnancy and lactation
Pregnancy
Pregnancy Category B
Reproduction studies have been performed in mice and rats at doses up to 40 times the human dose and have revealed no evidence of harm to the fetus due to cefixime. There are no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed.
Labor and Delivery
Cefixime has not been studied for use during labor and delivery. Treatment should only be given if clearly needed.
Nursing Mothers
It is not known whether cefixime is excreted in human milk. Consideration should be given to discontinuing nursing temporarily during treatment with this drug.
4.7. Effects on ability to drive and use machines
In the case of side effects such as encephalopathy (which may include convulsion, confusion, impairment of consciousness, movement disorders), the patient should not operate machines or drive a vehicle.
4.8. Undesirable effects
The most commonly seen adverse reactions were gastrointestinal events, which were reported in 30% of adult patients on either the twice-daily or the once-daily regimen. Clinically mild gastrointestinal side effects occurred in 20% of all patients, moderate events occurred in 9% of all patients and severe adverse reactions occurred in 2% of all patients.
Individual adverse reactions included diarrhoea (16%), loose or frequent stools (6%), abdominal pain (3%), nausea (7%), dyspepsia (3%), and flatulence (4%). Diarrhoea has been more commonly associated with higher doses. Other gastrointestinal side effects seen less frequently are vomiting and flatulence. Pseudomembranous colitis has been reported.
Acute generalized exanthematous pustulosis has been reported with Cefixime use in India.
The following adverse reactions have been reported following the post-approval use of cefixime. Incidence rates were less than 1 in 50 (less than 2%).
Gastrointestinal: Diarrhea, loose stools, abdominal pain, dyspepsia, nausea, and vomiting, pseudomembranous colitis
Hypersensitivity Reactions: Anaphylactic/anaphylactoid reactions (including shock and fatalities), skin rashes, urticaria, drug fever, pruritus, angioedema, and facial edema. Erythema multiforme, Stevens-Johnson syndrome, and serum sickness-like reactions have been reported;
Hepatic: Transient elevations in SGPT, SGOT, alkaline phosphatase, hepatitis, jaundice; Renal : Transient elevations in BUN or creatinine, acute renal failure; Central Nervous System : Headaches, dizziness, seizures;
Hemic and Lymphatic Systems: Transient thrombocytopenia, leukopenia, neutropenia, and eosinophilia. Prolongation in prothrombin time was seen rarely;
Abnormal Laboratory Tests: Hyperbilirubinemia;
Other: Genital pruritus, vaginitis, candidiasis, toxic epidermal necrolysis. In addition to the adverse reactions listed above which have been observed in patients treated with cefixime, the following adverse reactions and altered laboratory tests have been reported for cephalosporin-class antibiotics:
Adverse reactions: Allergic reactions, superinfection, renal dysfunction, toxic nephropathy, hepatic dysfunction including cholestasis, aplastic anemia, hemolytic anemia, haemorrhage and colitis. Several cephalosporins have been implicated in triggering seizures, particularly in patients with renal impairment when the dosage was not reduced. If seizures associated with drug therapy occur, the drug should be discontinued. Anticonvulsant therapy can be given if clinically indicated.
Abnormal Laboratory Tests: Positive direct Coombs test, elevated LDH, pancytopenia, agranulocytosis.
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via email to:medico@zuventus.com
Website: https://www.zuventus.com/drug-safety-reporting
By reporting side effects, you can help provide more information on the safety of this medicine.
4.9.Overdose
There is a risk of encephalopathy in cases of administration of beta-lactam antibiotics, including cefixime, particularly in case of overdose or renal impairment.
Adverse reactions seen at dose levels up to 2 g cefixime in normal subjects did not differ from the profile seen in patients treated at the recommended doses. Cefixime is not removed from the circulation in significant quantities by dialysis.
No specific antidote exists. General supportive measures are recommended.
5.0 Pharmacological properties
5.1 Pharmacodynamic properties
Mechanism of Action
Pharmacotherapeutic group: third generation cephalosporin, ATC code: J01DD08
Cefixime is an oral third generation cephalosporin which has marked in vitro bactericidal activity against a wide variety of Gram-positive and Gram-negative organisms.
Clinical efficacy has been demonstrated in infections caused by commonly occurring pathogens including Streptococcus pneumoniae, Streptococcus pyogenes, Escherichia coli, Proteus mirabilis, Klebsiella species, Haemophilus influenzae (beta-lactamase positive and negative), Branhamella catarrhalis (beta-lactamase positive and negative) and Enterobacter species. It is highly stable in the presence of beta-lactamase enzymes.
Most strains of enterococci (Streptococcus faecalis, group D Streptococci) and Staphylococci (including coagulase positive and negative strains and methicillin-resistant strains) are resistant to cefixime. In addition, most strains of Pseudomonas, Bacteroides fragilis, Listeria monocytogenes and Clostridia are resistant to cefixime.
5.2 Pharmacokinetic properties
Absorption
The absolute oral bioavailability of cefixime is in the range of 22 to 54%. Cefixime tablets and suspension, given orally, are about 40 to 50% absorbed whether administered with or without food; however, time to maximal absorption is increased approximately 0.8 hours when administered with food. Typically, the peak serum levels following the recommended adult or paediatric doses are between 1.5 and 3 mcg/ml. A single 200 mg tablet of cefixime produces an average peak serum concentration of approximately 2 mcg/mL(range: 1 to 4 mcg/mL). The oral suspension produces average peak concentrations approximately 25 to 50% higher than the tablets, when tested in normal adultvolunteers. Oral suspension 200 mg doses produce average peak concentrations of 3 mcg/mL (range: 1 to 4.5 mcg/mL), when tested in normal adult volunteers. The area under the time versus concentration curve (AUC) is greater by approximately 10 to 25% with the oral suspension than with the tablet after doses of 100 to 400 mg, when tested in normal adult volunteers. This increased absorption should be taken into consideration if the oral suspension is to be substituted for the tablet. Because of the lack of bioequivalence, tablets should not be substituted for oral suspension in the treatment
of otitis media. Crossover studies of tablet versus suspension have not been performed in children.
Absorption is not significantly modified by the presence of food. Cefixime may, therefore, be given without regard to meals. Peak serum concentrations occur between 2 and 6 hours following oral administration of a single 200 mg tablet, a single 400 mg tablet, or 400 mg of cefixime suspension. Peak serum concentrations occur between 2 and 5 hours following a single administration of 200 mg of suspension.
From in vitro studies, serum or urine concentrations of 1 mcg/ml or greater were considered to be adequate for most common pathogens against which cefixime is active.
Distribution
Cefixime is almost exclusively bound to the albumin fraction, the mean free fraction being approximately 30%. Serum protein binding is concentration independent, with a bound fraction of approximately 65%. Protein binding of cefixime is only concentration-dependent in human serum at very high concentrations, which are not seen following clinical dosing. In a multiple-dose study conducted with a research formulation, which is less bioavailable than the tablet or suspension, there was little accumulation of drug in serum or urine after dosing for 14 days.
Metabolism and Excretion
There is no evidence of metabolism of cefixime in vivo. Approximately 50% of the absorbed dose is excreted unchanged in the urine in 24 hours. Glomerular filtration is considered the predominant mechanism. Metabolites of cefixime have not been isolated from human serum or urine. In animal studies, it was noted that cefixime is also excreted in the bile in excess of 10% of the administered dose. The serum half-life of cefixime in healthy subjects is independent of dosage form and averages 3 to 4 hours, but may range up to 9 hours in some normal volunteers.
Special Populations
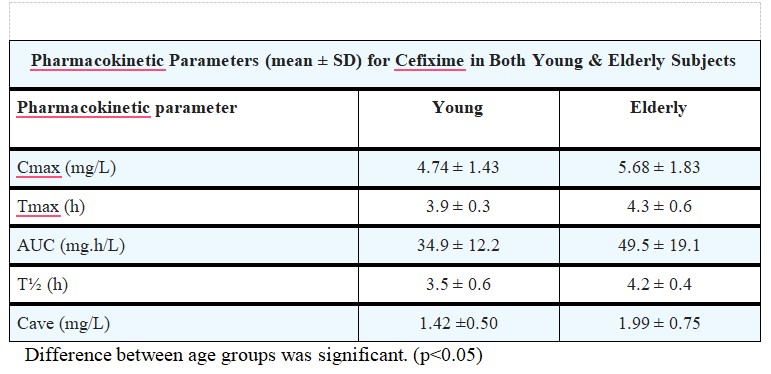
Geriatrics
Average AUCs at steady state in elderly patients are approximately 40% higher than average AUCs in other healthy adults. Differences in the pharmacokinetic parameters between 12 young and 12 elderly subjects who received 400 mg of cefixime once daily for 5 days are summarized as follows: Pharmacokinetic Parameters (mean ± SD) for Cefixime in Both Young & Elderly Subjects
Renal Impairment:
In subjects with moderate impairment of renal function (20 to 40 mL/min creatinine clearance), the average serum half-life of cefixime is prolonged to 6.4 hours. In severe renal impairment (5 to 20 mL/min creatinine clearance), the half-life increased to an average of 11.5 hours. The drug is not cleared significantly from the blood by hemodialysis or peritoneal dialysis. However, a study indicated that with doses of 400 mg, patients undergoing hemodialysis have similar blood profiles as subjects with creatinine clearances of 21 to 60 mL/min.
6.0 Nonclinical properties
There are no pre-clinical data of relevance to the prescriber which are additional to that already included in other sections of the Summary of Product Characteristics.
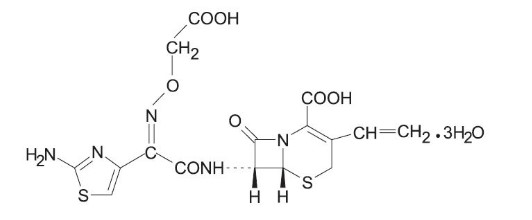
7.0 Description
Cefixime is a semisynthetic, cephalosporin antibacterial for oral administration. Chemically, it is (6R,7R)-7-[2-(2-Amino-4-thiazolyl)glyoxylamido]-8-oxo-3-vinyl-5-thia-1-azabicyclo [4.2.0] oct-2-ene-2-carboxylic acid, 72-(Z)-[O-(carboxy methyl) oxime] trihydrate.
Molecular weight = 507.50 as the Trihydrate.
Chemical Formula is C16H15N5O7S2.3H2O
The structural formula for cefixime is:
8.0 Pharmaceutical particulars
1.Incompatibilities
Not applicable.
2.Shelf-life
Refer on the pack.
3.Packaging information
C Tax-O 100 DT: A Strip of 10 tablets.
C Tax-O 200: A Strip of 10 tablets.
4.Storage and handing instructions
C Tax-O 100 DT: Store protected from moisture at a temperature not
exceeding 25°C. C Tax-O 200: Store in a cool & dry place. Protect from light. Keep out of reach of children.
9.0 Patient counselling information
Counsel patients that antibacterial drugs, including cefixime, should only be used to treat bacterial infections. They do not treat viral infections (e.g., the common cold). When cefixime is prescribed to treat a bacterial infection, patients should be told that although it is common to feel better early in the course of therapy, the medication should be taken exactly as directed. Skipping doses or not completing the full course of therapy may: (1) decrease the effectiveness of the immediate treatment and (2) increase the likelihood that bacteria will develop resistance and will not be treatable by cefixime tablets or other antibacterial drugs in the future.
Advise patients that diarrhea is a common problem caused by antibacterial drugs which usually ends when the antibacterial drug is discontinued. Sometimes after starting treatment with antibacterial drugs, patients can develop watery and bloody stools (with or without stomach cramps and fever) even as late as two or more months after having taken the last dose of the antibacterial drug. If this occurs, patients should contact their physician as soon as possible.
12.0 Date of revision
18th Sept. 2024
About leaflet
Read all of this leaflet carefully before you are given this medicine because it contains important information for you.
Keep this leaflet. You may need to read it again. If you have any further questions, ask your doctor, pharmacist or nurse. This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. If you get any side effects, talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4.
What is in this leaflet
- What C Tax-O tablets is and what it is used for
- What you need to know before you take C Tax-O tablets
- How to take C Tax-O tablets
- Possible side effects
- How to store C Tax-O tablets
- Contents of the pack and other information
1. What C Tax-O tablets is and what it is used for
C Tax-O tablets contains a medicine called Cefixime. This belongs to a group of antibiotics called ‘cephalosporins’.
C Tax-O tablets is used to treat infections caused by bacteria. These include infections of the:
- Ear
- Nose, sinuses (such as sinusitis)
- Throat (such as tonsillitis, pharyngitis)
- Chest and lungs (such as bronchitis, pneumonia)
- Urinary system (such as cystitis and kidney infections)
2. What you need to know before you are given C Tax-O tablets
Do not take C Tax-O tablets if:
- You are allergic to cefixime, any other cephalosporin antibiotics including penicillin or to any of the other ingredients of this medicine (listed in section 6).
- Signs of an allergic reaction include: a rash, swallowing or breathing problems, swelling of the lips, face, throat and tongue.
- Do not take this medicine if the above applies to you.
If you are not sure, talk to your doctor or pharmacist before taking C Tax-O tablets.
Warnings and precautions
Talk to your doctor or pharmacist or nurse before you are given C Tax-O tablets if:
- You have ever had colitis.
- You have kidney problems
If you are not sure if any of the above apply to you, talk to your doctor or pharmacist before taking this medicine. Severe skin problems such as Toxic Epidermal Necrolysis (TEN), Stevens-Johnson Syndrome (SJS), Drug Rash with Eosinophilia and Systemic Symptoms (DRESS), and Acute Generalised Exanthematous Pustulosis (AGEP) have been reported with cefixime (see section 4). If you develop severe skin reactions or any of the reactions listed in section 4, stop treatment immediately and contact your doctor or healthcare professional.
Other medicines and C Tax-O tablets
- Tell your doctor or pharmacist if you are taking, have recently taken or might take any other medicines. This includes medicines you buy without a prescription, including herbal medicines. This is because C Tax-O tablets can affect the way some other medicines work. Also, some medicines can affect the way C Tax-O tablets works.
- In particular, tell your doctor if you are taking the following:
- Medicines to thin the blood such as warfarin
Pregnancy and breast-feeding
If you are pregnant or breast-feeding, think you may be pregnant or are planning to have a baby, ask your doctor or pharmacist for advice before taking this medicine.
Driving and using machines
This medicine can cause symptoms including fits (convulsions), feeling confused, feeling less alert or aware of things than usual, unusual muscle movements or stiffness. If you experience any of these effects don’t drive or use machinery.
Medical Tests
If you require any tests (such as blood or urine tests) while taking this medicine, please make sure your doctor knows that you are taking C Tax-O tablets.
3. How to take C Tax-O tablets
Always use this medicine exactly as your doctor has told you. Check with your doctor or pharmacist if you are not sure.
C Tax-O tablets 200 mg Tablets:
- Take this medicine by mouth.
- Swallow tablets whole with a drink of water.
C Tax-O tablets 100 mg Dispersible tablets:
- Disperse the tablet in one teaspoonful (5 ml) of previously boiled & cooled water before administration.
If you feel the effect of the medicine is too weak or too strong, do not change the dose yourself, but ask your doctor. Carefully read the label from the pharmacist. Ask your pharmacist if you are not sure about the dose to take. The medicine should be taken for the prescribed number of days. The recommended dose is:
Adults, Elderly and Children over 10 years or weighing more than 50kg
- 200 mg – 400 mg each day given as a single or divided dose
People with kidney problems
- Your doctor may prescribe a lower dose.
Pediatric population (6 months or older)
- The recommended dose for C Tax-O DT is 8 mg/kg/day. This may be administered as a single daily dose or may be given in two divided doses, as 4 mg/kg every 12 hours.
- Children weighing more than 45 kg or older than 12 years should be treated with the recommended adult dose, 200 to 400 mg daily depending on the severity of infection.
If you take more C Tax-O tablets than you should
- If you have too much of this medicine, talk to your doctor straight away.
If you forget to take C Tax-O tablets
- If you forget to take a dose, take it as soon as you remember it. However, if it is nearly time for the next dose, skip the missed dose. Do not take a double dose to make up for a forgotten dose.
If you stop taking C Tax-O tablets
- Do not stop taking this medicine without talking to your doctor. You should not stop taking C Tax-O tablets just because you feel better. This is because the infection may come back or get worse again. If you have any further questions on the use of this medicine, ask your doctor or pharmacist.
4. Possible side effects
Like all medicines, this medicine can cause side effects, although not everybody gets them. Tell your doctor straight away or go to the nearest hospital casualty department if you notice any of the following serious side effects – you may need urgent medical treatment:
You have an allergic reaction. The signs may include: a rash, joint pain, swallowing or breathing problems, swelling of your lips, face, throat or tongue.
SJS/TEN symptoms may include blistering, peeling or bleeding on any part of the skin (including the lips, eyes, mouth, nose, genitals, hands or feet). Also, flu-like symptoms such as fever, chills or aching muscles.
DRESS symptoms may include flu-like symptoms and a widespread rash with a high body temperature and enlarged lymph nodes. Abnormal blood test results may include increased levels of liver enzymes and an increase in a type of white blood cell (eosinophilia) and enlarged lymph nodes.
AGEP symptoms may include a red, scaly, widespread rash with bumps under the skin (including your skin folds, chest, abdomen (including stomach), back and arms) and blisters accompanied by fever.
Erythema multiforme symptoms include skin rash or skin lesions with a pink/red ring and a pale centre which may be itchy, scaly or filled with fluid. The rash may appear especially on the palms or soles of your feet.
You get infections more easily than usual. This could be because of a blood disorder. This normally gets better after stopping the medicine.
You bruise or bleed more easily than normal. This could be because of a blood disorder. This normally gets better after stopping the medicine.
If your child gets nose bleeds, bleeding gums, chills, tiredness, pale skin (often with a yellow tinge), shortness of breath. This may be due to haemolytic anaemia.
Changes in the way the kidneys are working or blood in your child’s urine. Fits (convulsions)
A brain condition with symptoms including fits (convulsions), feeling confused, feeling less alert or aware of things than usual, unusual muscle movements or stiffness. This may be something called encephalopathy. This side effect is more likely if you have taken an overdose or you already have a problem with your kidneys.
Stop taking this medicine and contact your doctor without delay if you get:
- Severe watery diarrhoea that will not stop and you are feeling weak and have a fever. This may be something called ‘Pseudomembranous colitis’.
Tell your doctor or pharmacist if any of the following side effects get serious or lasts longer than a few days:
Feeling sick (nausea) or being sick (vomiting)
Stomach pains, indigestion or wind
Headaches
Feeling dizzy
Feeling itchy in the genital or vaginal area
Blood tests
C Tax-O tablets can cause blood clots or small changes to the way the liver and kidney work. This would be shown up in blood tests. This is not common and goes back to normal after stopping this medicine.
Reporting of side effects
If you get any side effects, talk to your doctor. This includes any possible side effects not listed in this leaflet. You can also report side effects directly: Website: www.zuventus.co.in and click the tab “Safety Reporting” located on the top of the home page. By reporting side effects, you can help provide more information on the safety of this medicine.
5. How to store C Tax-O tablets
Keep this medicine out of the sight and reach of children. Do not use this medicine after the expiry date which is stated on the label and blister pack after EXP. Store below 25°C. Do not throw away medicines via wastewater or household waste. Ask your pharmacist how to throw away medicines you no longer use. These measures will help protect the environment.
6. Contents of the pack and other information
What C Tax-O tablets contains
Each film coated C Tax-O tablets 200 mg tablet contains:
Cefixime IP (as Trihydrate) equivalent to
Cefixime (Anhydrous) 200 mg
Excipients q.s.
Colour: Titanium Dioxide IP
Each uncoated C Tax-O tablets 100 mg dispersible tablet contains:
Cefixime IP (as Trihydrate) equivalent to
Cefixime (Anhydrous) 100 mg
Excipients q.s.
Colour: Lake of Quinoline Yellow
Flavour added
Packing information:
C Tax-O tablets 100 DT: A strip of 10 tablets.
C Tax-O tablets 200: A strip of 10 tablets.
Marketing Authorisation Holder
Zuventus Healthcare Limited
Zuventus House, Plot Y2, CTS No.: 358/A2,
Near Nahur Railway Station,
Nahur (W), Mumbai, 400078 Maharashtra, India